Head-to-head: Zone 2 vs. Zone 3 frozen elephant trunk
Abstract
Total arch replacement via frozen elephant trunk (FET) is a strategy for managing complex thoracic aortic pathologies involving the arch and descending thoracic aorta (DTA). The FET procedure involves the distal anastomosis of the FET hybrid prosthesis at a chosen aortic arch zone. Though distal anastomosis has been traditionally performed at Zone 3 (Z-3-FET) of the aortic arch, recent practice has seen a significant increase in Zone 2 FET (Z-2-FET). The literature concerning independent Zone 2 and 3 studies and head-to-head comparative studies suggest that Z-2-FET is the superior approach, yielding more favourable results overall, except for aortic remodelling. The improved clinical outcomes achieved with Z-2-FET can be attributed to the shorter operative times, including cardiopulmonary bypass duration, due to the ease and increased surgical site exposure at the aortic arch using this technique. The slightly inferior aortic remodelling observed in Z-2-FET can be explained by the decreased coverage of the DTA distally by the FET stent graft. However, this difference in results can also be attributed to the complexity and severity of the underlying pathology and the surgical approach adopted. The prospect of utilising Zone 0 FET (Z-0-FET) is highly promising, with some studies hinting at its superiority over Z-2-FET. Nevertheless, studies are needed to determine the efficacy of Z-0-FET and directly compare it to Z-2-FET to reach a definitive consensus on the most optimal FET technique. The present literature review aims to provide an overview of major intraoperative and postoperative outcomes achieved with Z-2-FET and Z-3-FET and summarise evidence from studies directly comparing them. Another aim of this narrative review is to explore current literature trends on Z-0-FET uptake.
Keywords
INTRODUCTION
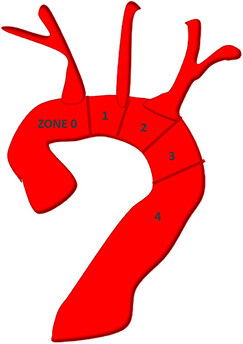
Total arch replacement (TAR) via frozen elephant trunk (FET) is a strategy for managing complex thoracic aortic pathologies involving the arch and descending thoracic aorta (DTA). Since its introduction, FET has revolutionised the field of aortovascular surgery by achieving superior results to conventional arch repair techniques, leading to its continuously increasing uptake. FET hybridises an “open-repair” approach with endovascular techniques. The stented ‘frozen’ distal elephant trunk segment, introduced into the DTA, also allows for a single-stage procedure. The FET surgical technique involves anastomosis of the distal cuff of the FET hybrid prosthesis (HP) to the native DTA wall at a chosen aortic arch zone[1,2]. The aortic arch zones are defined according to anatomical classifications established by Mitchell and Ishimaru[3] [Figure 1]. Though the distal anastomosis was traditionally performed at Zone 3 (Z-3-FET) of the aortic arch, there is debate on whether adopting Zone 2 (Z-2-FET) implantation improves surgical access and clinical outcomes[1,2]. As illustrated in Figure 1, Zone 2 involves the aortic arch between the left common carotid artery (LCCA) and the left subclavian artery (LSA), while Zone 3 involves the proximal DTA distal to the LSA. It is also possible that the re-intervention rates secondary to a new distal stent graft-induced entry tear, aortic dilatation, and endoleak will decline when the most appropriate FET HP type, size and length are used with a more proximalised distal anastomosis site[4-6]. Nevertheless, it is essential to note that clinical outcomes with Z-2-FET and Z-3-FET can be influenced by the complexity and severity of the underlying pathology and the surgical technique adopted for supra-aortic vessel re-implantation, intraoperative perfusion, and cerebral protection. There is additional debate on whether proximalisaton of the distal anastomosis to Zone 0 of the arch will optimise outcomes[7]. The current literature review aims to provide an overview of major intraoperative and postoperative clinical outcomes of Z-2-FET and Z-3-FET, with a focus on studies that explicitly compare results of Z-2-FET and Z-3-FET head-to-head, including operative times, mortality, neurological complications, recurrent laryngeal nerve injury, respiratory and renal outcomes, haemostasis, and aortic remodelling. Another scope of this review is to explore current literature trends in the uptake of Zone 0 FET (Z-0-FET).
Figure 1. Illustration depicting the aortic arch’s different Zones (0-4). Original figure. Reused from Choudhury et al.[1].
ZONE 2 FROZEN ELEPHANT TRUNK
Z-2-FET technicalities
Z-2-FET implantation involves resection of the diseased aortic arch up to the area distal to the LCCA but proximal to the origin of the LSA. Following resection and inspection of the remaining distal arch and DTA, the stent graft can be introduced over the femoral guide wire (if used) into the true lumen and anastomosed, with caution to ensure residual LSA patency. As aforementioned, emerging evidence over the past decade has supported this “proximalised” approach to TAR with FET: beyond Zone 2, the distal arch and DTA sit relatively deep and posterior within the chest cavity, making distal resection, inspection, and anastomosis more challenging[1,8]. Zone 2 implantation is, therefore, likely to involve decreased visceral circulatory arrest and cardiopulmonary bypass (CPB) durations, which are changes that may reflect improved clinical outcomes. Various Z-2-FET techniques for supra-aortic vessel implantation and LSA revascularisation exist, the choice of which can influence results.
Overview of clinical outcomes with Z-2-FET
The increasing popularity of Zone 2 distal anastomosis in FET is manifested in the recent data demonstrating its efficacy. The Pennsylvania group achieved successful thoracic false lumen (FL) obliteration in 80% of cases, with 17% complete thromboses[9]. Findings from Chen et al. echo this success, with three-month computed tomography surveillance showing FL obliteration in 91.7% of acute DeBakey 1 dissections[10].More recent data from a Chinese single-centre study showed similar positive results, with FL thrombosis confirmed on imaging in 92.3% of patients treated for acute type B dissection (TBAD)[11]. In their 148-patient series, Sun et al. reported an in-hospital mortality of 4.7% for patients undergoing Z-2-FET for type A aortic dissection (TAAD), with 99% of lesions remaining free from reoperation[12]. Other series have been described equally as encouraging success, while groups in Japan and China have reported zero deaths in their studies[11,13]. Generally, the mortality rates in the literature range from 4.2%-14.3%[9,10,12,14-19].
Upon searching independent Z-2-FET studies within the literature, neurological outcomes were similarly encouraging, with numerous studies reporting zero incidences of clinically relevant spinal cord injury (SCI)[15,17,19]. However, more extensive series, including that from the Bologna group[20], have described the incidence of spinal cord injuries at about 5%. Stroke, however, remains a significant potential complication of FET, with the reported postoperative rates being 1.9%-10.7%[9-15,17,18]. Augmentations to surgical techniques and neuroprotective protocols are expected to ameliorate these neurological outcomes. Factors beyond the distal anastomosis site will influence clinical practice’s neurological and mortality/morbidity outcomes. Significant factors are the complexity and severity of the underlying pathology and the surgical approach adopted (supra-aortic vessel re-implantation and LSA revascularisation).
ZONE 3 FROZEN ELEPHANT TRUNK
Z-3-FET technicalities
The surgical approach in Z-3-FET involves a deeper aortic arch resection distal to the origin of LSA. Manipulation of the arch at Zone 3 poses more technical challenges due to its anatomic position deep within the chest[1]. Furthermore, FET implantation at Zone 3 requires a more extensive dissection of surrounding structures, which increases the risk of inadvertent damage to the recurrent laryngeal nerve (RLN)[21]. Similar to Z-2-FET, different surgical approaches to Z-3-FET for re-implantation of the supra-aortic vessels exist[1]. However, increased surgical complexity associated with Z-3-FET precipitates longer hypothermic circulatory arrest and CPB durations, which may increase the risk of neurological injury, visceral ischaemia, and renal complications[7]. Nevertheless, it is essential to note that the choice of the Z-3-FET technique can reflect in the results observed.
Overview of clinical outcomes with Z-3-FET
Mortality rates reported in small independent Z-3-FET studies are comparable to Z-2-FET but are challenged in studies of larger sample sizes. A 32-patient series by Hoffman et al. reporting on FET for acute TAAD found 30-day and 6-month mortality rates of 0% and 3.1%, respectively[22]. Similarly, favourable results for acute TBAD were seen by Kreibich et al., who reported no deaths[23]. However, more extensive independent studies have demonstrated early postoperative mortality rates ranging from 6%-15.3%[24-27].
There appears to be a modest variation in reported Z-3-FET neurological outcomes. The incidence of SCI was 7.4% in the 2019 single-centre study of 68 patients from the Heidelberg group[27]. On the other hand, and surprisingly, some series did not report SCI as a complication[22,23,25]. The same group also reported a combined incidence of postoperative stroke of 10.3% in their pooled acute and chronic aortic pathology cohort. The variability in neurological complications is apparent in Goebel et al., which reported a much lower stroke rate of 2.8%, and in a couple of studies observing no postoperative strokes[22-24]. The literature has substantial heterogeneity in preoperative patient characteristics and intraoperative factors, including the exact FET device, deployed and surgical technique used. Furthermore, not all series delineate the precise surgical technique relevant to our purposes, thus limiting the scope of potentially relevant data. Therefore, FET studies must incorporate neurological outcomes into their results in addition to unambiguous identification of the aortic arch zone adopted for FET HP distal anastomosis.
HEAD-TO-HEAD: ZONE 2 vs. ZONE 3 FET
The direct comparison of Z-2-FET and Z-3-FET is challenging as they are ultimately distinct procedures that vary according to surgical preference and the aortic anatomy of individual patients. There is also a paucity of evidence in studies that directly compare Z-2-FET and Z-3-FET intraoperative and postoperative outcomes, including operative times, mortality, neurological complications, RLN injury, respiratory and renal outcomes, haemostasis, and aortic remodelling. However, contemporary practice has seen an increased uptake of Z-2-FET due to reduced operative times [Table 1] and a lower risk of postoperative complications[8,21,28-32] [Table 2].
Comparison of devices and intra-operative outcomes observed across recent Z-2-FET and Z-3-FET comparison studies
| Study | Year | Sample Size Distribution | Devices used | Cardiopulmonary bypass time (mins) | Cerebral perfusion time (mins) | Circulatory/cardioplegic arrest time (mins) | Visceral ischemia time (mins) | ||||||
| Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | ||
| Detter et al.[29] n = 92 | 2019 | n = 30 TAA: 50% CAD: 43% AAD: 7% | n = 62 AAD: 37% TAA: 32% CAD: 31% | Thoraflex (100%) | Thoraflex (82%) E-Vita (18%) | - | - | 60.9 SD: ± 13.5 | 92.1*** SD: ± 33.1 | 41.7 SD: ± 10.5 Circulatory | 76.5*** SD: ± 33.0 Circulatory | - | - |
| Leone et al.[8] n = 282 | 2019 | n = 69 CAD: 55% AAD: 30% TAA: 15% | n = 213 CAD: 59% TAA: 29% AAD: 11% | E-Vita (59%) Thoraflex (41%) | 200 IQR: 126-658 | 210 IQR: 121-534 | 91 IQR: 30-294 | 88 IQR: 30-281 | - | - | 42 IQR: 25-106 | 54 IQR: 22-109 | |
| Panfilov et al.[31] n = 43 | 2021 | n = 17 | n = 27 | E-Vita (100%) | 188 IQR: 153-216 | 227 IQR: 199-256 | 57 IQR: 37-91 | 59.5 IQR: 53-69 | 35 IQR: 27-45 Circulatory | 50.5 IQR: 31-62 Circulatory | - | - | |
| Tsagakis et al.[28,32] n = 286 | 2018 | n = 183 | n = 103 | E-vita (100%) | 231** SD: ± 51 | 250 SD: ± 61 | 56*** SD: ± 14 | 68 SD: ± 18 | 125*** SD: ± 38 Cardioplegic | 147 SD: ± 33 Cardioplegic | 39*** SD: ± 16 | 70 SD: ± 24 | |
| Jakob et al.[21] † n = 135 | 2017 | n = 40 | n = 95 | E-vita (100%) | 254 SD: ± 52 | 252 SD: ± 61 | 57*** SD: ± 13 | 68 SD: ± 18 | 126** SD: ± 43 Cardioplegic | 147 SD: ± 35 Cardioplegic | 59*** SD: ± 15 | 72 SD: ± 23 | |
Comparison of postoperative outcomes observed across recent Z-2-FET and Z-3-FET comparison studies
| Paper | 30-day mortality (%) | Paraplegia (%) | Permanent Stroke (%) | Recurrent nerve injury (%) | Respiratory complication (%) | Renal failure/dialysis (%) | Reoperation for bleeding (%) | |||||||
| Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | Z-2-FET | Z-3-FET | |
| Detter et al.[29] Z-2; n = 30 Z-3; n = 62 | 3.3 | 17.7 | 0 | 1.6 | 0 | 17.7* | 3.3 | 22.6* | - | - | 13.3 | 17.7 | 3.3 | 17.7 |
| Leone et al.[8] Z-2; n = 69 Z-3; n = 213 | 20^ | 16^ | 0 | 4.7 | 5.8 | 9.9 | 2.8 | 5.2 | 11.6 | 7.5 | 14.5 | 20.7 | 12.2† | 15.9† |
| Panfilov et al.[31] Z-2; n = 17 Z-3; n = 27 | 9.1 | 9.1 | 5.9 | 0 | 5.9 | 3.7 | - | - | 47.1 | 40.7 | 29.4 | 25.9 | 0 | 11.1 |
| Tsagakis et al.[28] Z-2; n = 183 Z-3; n = 103 | 11 | 11 | 2 | 4 | 4 | 8 | - | - | 19 | 42** | 26 | 43** | - | - |
| Tsagakis et al.[32] Z-2; n = 204 Z-3; n = 103 | 11.8 | 11.7 | 2 | 4.9 | 6.4 | 8.7 | - | - | 28.4 | 52.4*** | 26 | 39.8 * | 8.3 | 14.6 |
Intraoperative outcomes
CPB and cerebral perfusion
CPB and cerebral perfusion times are lower with Z-2-FET[8,28,29,31,32]. Leone et al. reported a CPB time of 200 min achieved with Z-2-FET (n = 69) vs. 210 min with Z-3-FET (n = 213) (P = 0.171)[8]. Similarly, but with a more pronounced difference in CPB times, Panfilov et al. recorded 188 min in their Z-2-FET group (n = 17) vs. 227 min in the Z-3-FET group (n = 27) (P = 0.013)[31]. The overall retrospective analysis of data captured between 2005-2018 by the Essen group showed 231 min of CPB achieved with ≤ Z-2-FET (n = 204) vs. 250 min in Z-3-FET (n = 103) (P < 0.001)[32]. Cerebral perfusion time was also lower at 56 min with ≤ Z-2-FET compared to 65 min in the Z-3-FET cohort (P < 0.001)[32]. Detter et al. additionally demonstrated respective cerebral perfusion times of 61 min and 92 min (P < 0.001)[29]. Leone et al. and Panfilov et al. reported comparable cerebral perfusion durations between Z-2-FET and Z-3-FET of 91 vs. 88 min and 57 vs. 59.5 min, respectively[8,31].
Visceral ischaemia time
Since Z-2-FET procedures are technically more straightforward and less time intensive, this has resulted in lower visceral ischaemia times and risk of postoperative morbidity. Tsagakis and Jakob[32] recorded an average of 39 min of visceral ischaemia in their ≤ Z-2-FET cohort (n = 204) compared to 70 min in their Z-3-FET cohort (n = 103) (P < 0.001). It is possible that the inclusion of procedures (n = 19) performed more proximal than Z-2, attributed to the significantly lower visceral ischaemia time. In addition, cardioplegia time was also significantly less with Z-2-FET than with Z-3-FET (125 vs. 147 min, respectively;
Postoperative outcomes
Mortality
There appears to be an insignificant difference between Z-2-FET and Z-3-FET mortality rates only in the short and middle term. Leone et al. found an insignificant difference in in-hospital mortality between their Z-2-FET group (20%, n = 69) and their Z-3-FET (16%, n = 213) group (P = 0.518)[8]. Mortality is mainly represented as 30-day in the head-to-head studies. The 30-day mortalities in head-to-head studies suggest insignificant differences between Z-2-FET and Z-3-FET. For instance, 30-day mortalities were virtually equivalent in Tsagakis et al. and Panfilov et al. at 12% and 9%, respectively, for both FET groups in each[32,31]. Elsewhere, 3.3% of Z-2-FET patients in Detter et al. had died at 30 days relative to 17.7% with Z-3-FET, yet, this did not reach significance
Neurological outcomes
Neurological insult is a well-characterised complication associated with the aortic arch repair. There is a general trend towards a lower incidence of paraplegia in Z-2-FET patients[8,28,29]. Leone et al. and Tsagakis et al. reported post-Z-3-FET paraplegia incidence of ± 4.5% compared to 0% and 2%, respectively, achieved utilising Z-2-FET[8,28]. Similarly, Detter et al. observed fewer cases of paraplegia with Z-2-FET than with Z-3-FET (0% vs. 1.6%, respectively)[29]. The fact that 0% postoperative paraplegia is achieved with Z-2-FET is auspicious and reflects growing surgical expertise with the proximalised FET technique. A more distal proximal landing zone for the FET stent graft deployment has previously been identified as a major risk factor for ischaemic neurological injury[34], as have FET stents > 15 cm or those extending beyond T8[35]. On the contrary, a stent graft length < 10 cm may decrease the risk of SCI[35]. This is evident in one of the most extensive FET meta-analyses, which analysed neurological outcomes data from a total of 3154 patients from 35 studies and demonstrated that a 10 cm FET stent graft is protective against SCI compared to a 15 cm device (2.5% vs. 11.6%; P < 0.001)[36]. Stroke remains a concern with both Z-2-FET and Z-3-FET, although 0% stroke has been reported for Z-2-FET in the literature[29]. Available head-to-head studies demonstrate a permanent stroke rate of 0%-6% with Z-2-FET and between 4%-18% with Z-3-FET[8,28,29,31] [Table 2]. These more favourable results are likely due to less coverage of the distal thoracic aorta and its branching vertebral arteries and generally reduced ischaemic times achieved with Z-2-FET [Table 1]. Conversely, Panfilov et al. reported improved neurological outcomes with Z-3-FET[31]; however, this should be interpreted with caution based on the relatively small patient population studied.
RLN injury
The RLN loops under the aortic arch near Zones 2 and 3. Proximalisation of the surgical field improves access to the anastomosis sites and decreases the risk of RLN damage. Detter et al. reported RLN injury in only 3.3% of Z-2-FET patients compared to 22.6% of Z-3-FET patients (OR 0.17; 95%CI: 0.02-0.78;
Respiratory outcomes
Respiratory failure post-FET is a well-recognised cause of mortality and should be considered carefully alongside renal outcomes, given the intricately related physiology[37,38]. Two studies observed more than 40% respiratory failure rates with Z-3-FET[28,31]. However, it remains unclear whether respiratory outcomes are superior to Z-2-FET or Z-3-FET, as recent studies show heterogeneous results. Tsagakis et al. reported prolonged ventilation in 19% of Z-2-FET patients vs. 43% of the Z-3-FET group (P < 0.001)[28]. However, Leone et al. showed significantly higher rates of tracheostomy with Z-2-FET than Z-3-FET at 11.6% vs. 7.1%, respectively (P < 0.001)[8]. Similarly, Panfilov et al. outlined that a tracheostomy was needed in 47.7% of Z-2-FET patients and 40.7% of Z-3-FET patients, although the sample size in this study was possibly insufficient to bring to statistical significance (P = 0.419)[31].
Renal outcomes
Renal failure post-FET often necessitates temporary post-procedural dialysis. A 2020 systematic review by Tian et al. outlined a 15.5% rate (95%CI: 11.9-20.1) of acute kidney injury postoperatively across different aortic pathologies necessitating repair using FET[39]. A recent systematic review and meta-analysis by Rezaei et al. outlined that the positioning of the FET HP distal anastomosis at Zone 2 of the aortic arch was correlated with a significantly lower occurrence of renal failure compared to Z-3-FET (OR 0.52; 95%CI: 0.33-0.82; P = 0.069; I2 = 0%)[35]. This finding reflects the statistics outlined in Table 2, highlighting that most of the contemporary head-to-head evidence suggests superior renal outcomes with Z-2-FET. Tsagakis et al. demonstrated the most striking difference, who reported renal failure/dialysis of 26% with Z-2-FET vs. 43% with Z-3-FET (P = 0.004)[28]. This substantial difference can be attributed to the reduced ischaemic times in Z-2-FET achieved by LSA rerouting, as detailed elsewhere by this group[40]. Others have also demonstrated Z-2-FET renal failure/dialysis rates of 13.3%-14.5% compared to Z-3-FET rates of 17.7%-20.7%[8,29]. Intriguingly, Panfilov et al. reported that renal replacement therapy was needed in 29.4% of Z-2-FET patients vs. 25.9% of Z-3-FET patients (P = 0.833)[31]. However, it must be noted that their sample size
Haemostasis
Evidence in the literature suggests that Z-2-FET is associated with lower rates of bleeding requiring re-intervention compared to Z-3-FET. Longer CPB times, and associated physiological derangements, associated with Z-3-FET in the foreground of multiple vascular anastomoses offer a possible explanation[41]. To elaborate, Detter et al. found that 3.3% of the Z-2-FET group required re-sternotomy for bleeding/tamponade in comparison to 17.7% of their Z-3-FET group[29]. Similarly, Panfilov et al. achieved a 0% re-intervention rate for bleeding using Z-2-FET vs. 11.1% using Z-3-FET[31].
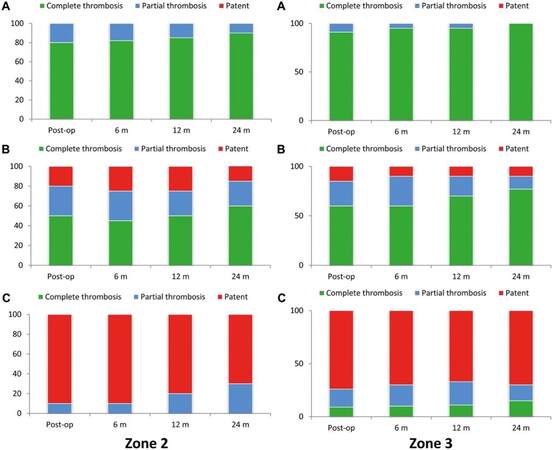
Aortic remodelling and FL thrombosis
Aortic remodelling refers to the process by which the aortic lumen returns to normality through expansion of the true lumen and regression of the FL through FL thrombosis. In their recent review, Jubouri et al. and Kayali et al. showcased the excellent aortic remodelling associated with FET[4,6]. Panfilov et al. is the only identified study directly comparing aortic remodelling achieved with Z-2-FET and Z-3-FET head-to-head[31]. The aorta was divided into three segments during follow-up radiological imaging to assess and compare remodelling. Segment A was the length along the FET HP; segment B was from the distal end of the stent graft down to the coeliac artery level; segment C was from the coeliac artery to the aortic bifurcation level. Figure 2 (reproduced from Panfilov et al.) represents the overall results[31]. The authors concluded that Z-3-FET is associated with improved aortic remodelling and FL thrombosis in the long term. This finding can be attributed to the extended coverage of the DTA distally by the FET stent graft in Z-3-FET[31].
Figure 2. FL thrombosis rate of patients in the Z-2-FET and Z-3-FET groups at the midterm follow-up. (A) Segment A; (B) segment B; and (C) segment C. Reproduced from Panfilov et al. with copyright permission obtained (from Oxford University Press)[31]. FET: frozen elephant trunk
ZONE 0 FROZEN ELEPHANT TRUNK
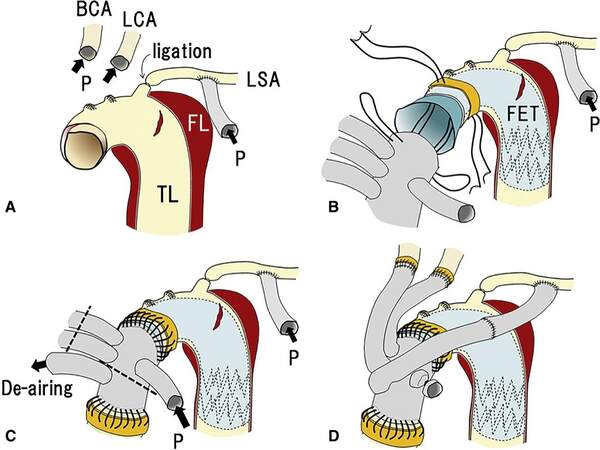
Recently, FET practice has shifted towards the proximalisation of the distal device anastomosis (or proximal landing zone of the stent graft) at Zone 0 of the aortic arch. The literature has hinted at this technique’s superiority over Z-2-FET regarding operative times and clinical outcomes[7]. The Z-0-FET can be performed using two main surgical techniques. The first is the hybrid arch repair, which requires debranching of the supra-aortic vessels, an example of which is illustrated in Figure 3[42,43]. The second uses FET HPs that facilitate Z-0-FET without time-consuming supra-aortic vessel debranching[44,45].
Figure 3. Detailed illustration of the Z-0-FET surgical technique. Reproduced from Yamamoto et al. with copyright permission obtained (Elsevier open access)[42]. BCA: Brachiocephalic artery; LCA: left carotid artery; P: perfusion; LSA: left subclavian artery; FL: false lumen; TL: true lumen; FET: frozen elephant trunk.
Yamamoto et al. presented their single-centre experience with Z-0-FET in 108 patients[42]. The 30-day and in-hospital mortality rates were 2.8% and 6.5%, respectively, with overall survival at 1, 2, and 3 years being 89.8%, 88.1%, and 88.1%, respectively. As for neurological outcomes, new-onset permanent neurological dysfunction and SCI occurred in 3.7% and 0% of patients, respectively[42].
Tan et al. recently published a literature review comparing Z-0-FET with Z-2-FET[7]. Using data from independent studies, the authors highlighted several clinical outcomes, including aortic remodelling, mortality, neurological injury, renal injury, RLN injury and re-intervention. Overall, Z-0-FET can be considered a superior solution for complex thoracic aortic disease, offering optimised results compared to Z-2-FET, except for aortic remodelling and FL thrombosis. This improvement in clinical outcomes can be attributed to the reduced operative times, including CPB duration, due to the more straightforward surgical access and the increased exposure of the anastomosis site. On the other hand, the decreased coverage of the DTA distally with Z-0-FET can explain the inferior aortic remodelling and FL thrombosis observed[7].
A solid conclusion on Z-0-FET’s superiority cannot be drawn at this stage since it is still relatively novel. In addition, Z-0-FET is not yet as well-established within the literature as Z-2-FET and Z-3-FET. Therefore, more studies investigating this potential paradigm-shifting technique are needed to reach a definitive consensus.
CONCLUSION
FET can be considered the primary choice for TAR due to its optimal clinical outcomes. Performing Z-2-FET seems to yield more favourable results than Z-3-FET, which can be attributed to the reduced operative times, including CPB duration, due to the ease and increased surgical site exposure at the aortic arch. The prospect of Z-0-FET is highly promising, but its superiority over Z-2-FET is yet to be proven.
DECLARATIONS
Authors’ contributionsDevised the manuscript topic and supervised the literature search and writing process: Bashir M
Performed the literature search: Jubouri M, Hussain K, Alzaanin W
Wrote the manuscript: Geragotellis A, Jubouri M, Tan SZCP
Provided feedback on the manuscript draft: Mohammed I, Bashir M
Edited and formatted the final version of the manuscript: Geragotellis A, Jubouri M
Approved this final version of the manuscript: Geragotellis A, Jubouri M, Hussain K, Alzaanin W, Tan SZCP, Patel R, Mohammed I, Bashir M
Availability of data and materialsThe data supporting this study’s findings are publicly available in electronic databases such as PubMed, Ovid, Google Scholar, Scopus and EMBASE.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2023.
REFERENCES
1. Choudhury RY, Basharat K, Zahra SA, et al. “Proximalization is Advancement”-Zone 3 frozen elephant trunk vs Zone 2 frozen elephant trunk: a literature review. Vasc Endovascular Surg 2021;55:612-8.
2. Mousavizadeh M, Bashir M, Jubouri M, et al. Zone proximalization in frozen elephant trunk: What is the optimal zone for open intervention? J Cardiovasc Surg (Torino) 2022;63:265-74.
3. Mitchell RS, Ishimaru S, Ehrlich MP, et al. First International Summit on Thoracic Aortic Endografting: roundtable on thoracic aortic dissection as an indication for endografting. J Endovasc Ther 2002;9:II98-105.
4. Jubouri M, Kayali F, Saha P, et al. Incidence of distal stent graft induced new entry vs. aortic remodeling associated with frozen elephant trunk. Front Cardiovasc Med 2022;9:875078.
5. Geragotellis A, Surkhi AO, Jubouri M, et al. Endovascular reintervention after frozen elephant trunk: where is the evidence? J Cardiovasc Surg (Torino) 2022;63:425-33.
6. Kayali F, Jubouri M, Tan SZ, Mohammed I, Bashir M. Aortic remodeling in aortic dissection after frozen elephant trunk: overcoming the challenges. J Cardiovasc Surg (Torino) 2022;63:434-8.
7. Tan SZCP, Lopuszko A, Munir W, Adams B, Bashir M. Aortic proximalization-Zone 0 vs. Zone 2: a concept or true challenge? J Card Surg 2021;36:3319-25.
8. Leone A, Di Marco L, Coppola G, et al. Open distal anastomosis in the frozen elephant trunk technique: initial experiences and preliminary results of arch Zone 2 versus arch Zone 3†. Eur J Cardiothorac Surg 2019;56:564-71.
9. Pochettino A, Brinkman WT, Moeller P, et al. Antegrade thoracic stent grafting during repair of acute DeBakey I dissection prevents development of thoracoabdominal aortic aneurysms. Ann Thorac Surg 2009;88:482-9;discussion 489.
10. Chen X, Huang F, Xu M, et al. The stented elephant trunk procedure combined total arch replacement for Debakey I aortic dissection: operative result and follow-up. Interact Cardiovasc Thorac Surg 2010;11:594-8.
11. Qi RD, Zhu JM, Liu YM, et al. Frozen elephant trunk for acute type B dissection involving the distal arch in the hybrid repair era. Ann Thorac Surg 2018;106:1182-8.
12. Sun L, Qi R, Zhu J, Liu Y, Zheng J. Total arch replacement combined with stented elephant trunk implantation: a new “standard” therapy for type a dissection involving repair of the aortic arch? Circulation 2011;123:971-8.
13. Koizumi S, Nagasawa A, Koyama T. Total aortic arch replacement using frozen elephant trunk technique with J Graft Open Stent Graft for distal aortic arch aneurysm. Gen Thorac Cardiovasc Surg 2018;66:91-4.
14. Tan SZCP, Jubouri M, Mohammed I, Bashir M. What is the long-term clinical efficacy of the thoraflex™ hybrid prosthesis for aortic arch repair? Front Cardiovasc Med 2022;9:842165.
15. Uchida N, Katayama A, Tamura K, Sutoh M, Kuraoka M, Ishihara H. Frozen elephant trunk technique and partial remodeling for acute type A aortic dissection. Eur J Cardiothorac Surg 2011;40:1066-71.
16. Shen K, Tang H, Jing R, Liu F, Zhou X. Application of triple-branched stent graft for Stanford type A aortic dissection: potential risks. Eur J Cardiothorac Surg 2012;41:e12-7.
17. Yamane Y, Uchida N, Mochizuki S, Furukawa T, Yamada K. Early- and mid-term aortic remodelling after the frozen elephant trunk technique for retrograde type A acute aortic dissection using the new Japanese J Graft open stent graft. Interact Cardiovasc Thorac Surg 2017;25:720-6.
18. Roselli EE, Idrees JJ, Bakaeen FG, et al. Evolution of simplified frozen elephant trunk repair for acute debakey type I dissection: midterm outcomes. Ann Thorac Surg 2018;105:749-55.
19. Hohri Y, Yamasaki T, Matsuzaki Y, Hiramatsu T. Early and mid-term outcome of frozen elephant trunk using spinal cord protective perfusion strategy for acute type A aortic dissection. Gen Thorac Cardiovasc Surg 2020;68:1119-27.
20. Di Bartolomeo R, Murana G, Di Marco L, et al. Is the frozen elephant trunk frozen? Gen Thorac Cardiovasc Surg 2019;67:111-7.
21. Jakob H, Dohle D, Benedik J, et al. Long-term experience with the E-vita Open hybrid graft in complex thoracic aortic disease†. Eur J Cardiothorac Surg 2017;51:329-38.
22. Hoffman A, Damberg ALM, Schälte G, Mahnken AH, Raweh A, Autschbach R. Thoracic stent graft sizing for frozen elephant trunk repair in acute type A dissection. J Thorac Cardiovasc Surg 2013;145:964-969.e1.
23. Kreibich M, Berger T, Morlock J, et al. The frozen elephant trunk technique for the treatment of acute complicated Type B aortic dissection. Eur J Cardiothorac Surg 2018;53:525-30.
24. Goebel N, Nagib R, Salehi-Gilani S, et al. One-stage hybrid aortic repair using the frozen elephant trunk in acute DeBakey type I aortic dissection. J Thorac Dis 2018;10:4195-203.
25. Berger T, Kreibich M, Morlock J, et al. True-lumen and false-lumen diameter changes in the downstream aorta after frozen elephant trunk implantation. Eur J Cardiothorac Surg 2018;54:375-81.
26. Shrestha M, Kaufeld T, Beckmann E, et al. Total aortic arch replacement with a novel 4-branched frozen elephant trunk prosthesis: Single-center results of the first 100 patients. J Thorac Cardiovasc Surg 2016;152:148-159.e1.
27. Kremer J, Preisner F, Dib B, et al. Aortic arch replacement with frozen elephant trunk technique - a single-center study. J Cardiothorac Surg 2019;14:147.
28. Tsagakis K, Wendt D, Dimitriou AM, et al. The frozen elephant trunk treatment is the operation of choice for all kinds of arch disease. J Cardiovasc Surg (Torino) 2018;59:540-6.
29. Detter C, Demal TJ, Bax L, et al. Simplified frozen elephant trunk technique for combined open and endovascular treatment of extensive aortic diseases. Eur J Cardiothorac Surg 2019;56:738-45.
30. Jakob H, Moughal S, Bashir M. Frozen elephant trunk with straight vascular prosthesis: single-center experience with a review of current trends. J Cardiovasc Surg (Torino) 2020;61:301-7.
31. Panfilov DS, Kozlov BN, Pryakhin AS, Kopeva KV. Frozen elephant trunk technique with different proximal landing zone for aortic dissection. Interact Cardiovasc Thorac Surg 2021;33:286-92.
32. Tsagakis K, Jakob H. Which frozen elephant trunk offers the optimal solution? Semin Thorac Cardiovasc Surg 2019;31:679-85.
33. Akbulut M, Ak A, Arslan O, et al. Comparison between arch zones in modified frozen elephant trunk procedure for complex thoracic aortic diseases. Braz J Cardiovasc Surg 2020;35:934-41.
34. Leontyev S, Tsagakis K, Pacini D, et al. Impact of clinical factors and surgical techniques on early outcome of patients treated with frozen elephant trunk technique by using EVITA open stent-graft: results of a multicentre study. Eur J Cardiothorac Surg 2016;49:660-6.
35. Rezaei Y, Bashir M, Mousavizadeh M, et al. Frozen elephant trunk in total arch replacement: a systematic review and meta-analysis of outcomes and aortic proximalization. J Card Surg 2021;36:1922-34.
36. Preventza O, Liao JL, Olive JK, et al. Neurologic complications after the frozen elephant trunk procedure: a meta-analysis of more than 3000 patients. J Thorac Cardiovasc Surg 2020;160:20-33.e4.
37. Ko GJ, Rabb H, Hassoun HT. Kidney-lung crosstalk in the critically ill patient. Blood Purif 2009;28:75-83.
38. Pierson DJ. Respiratory considerations in the patient with renal failure. Respir Care 2006;51:413-22.
39. Tian DH, Ha H, Joshi Y, Yan TD. Long-term outcomes of the frozen elephant trunk procedure: a systematic review. Ann Cardiothorac Surg 2020;9:144-51.
40. Tsagakis K, Dohle DS, Wendt D, et al. Left subclavian artery rerouting and selective perfusion management in frozen elephant trunk surgery. Minim Invasive Ther Allied Technol 2015;24:311-6.
41. Damberg A, Schälte G, Autschbach R, Hoffman A. Safety and pitfalls in frozen elephant trunk implantation. Ann Cardiothorac Surg 2013;2:669-76.
42. Yamamoto H, Kadohama T, Yamaura G, et al. Total arch repair with frozen elephant trunk using the “zone 0 arch repair” strategy for type A acute aortic dissection. J Thorac Cardiovasc Surg ;2019:36-45.
43. Hughes GC, Vekstein A. Current state of hybrid solutions for aortic arch aneurysms. Ann Cardiothorac Surg 2021;10:731-43.
44. Jakob H, Shehada SE, Dohle D, et al. New 3-zone hybrid graft: first-in-man experience in acute type I dissection. J Thorac Cardiovasc Surg 2022;163:568-574.e1.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Geragotellis A, Jubouri M, Hussain K, Alzaanin W, Tan SZCP, Patel R, Mohammed I, Bashir M. Head-to-head: Zone 2 vs. Zone 3 frozen elephant trunk. Vessel Plus 2023;7:6. http://dx.doi.org/10.20517/2574-1209.2022.41
AMA Style
Geragotellis A, Jubouri M, Hussain K, Alzaanin W, Tan SZCP, Patel R, Mohammed I, Bashir M. Head-to-head: Zone 2 vs. Zone 3 frozen elephant trunk. Vessel Plus. 2023; 7: 6. http://dx.doi.org/10.20517/2574-1209.2022.41
Chicago/Turabian Style
Geragotellis, Alexander, Matti Jubouri, Kamran Hussain, Waseem Alzaanin, Sven ZCP Tan, Ravi Patel, Idhrees Mohammed, Mohamad Bashir. 2023. "Head-to-head: Zone 2 vs. Zone 3 frozen elephant trunk" Vessel Plus. 7: 6. http://dx.doi.org/10.20517/2574-1209.2022.41
ACS Style
Geragotellis, A.; Jubouri M.; Hussain K.; Alzaanin W.; Tan SZCP.; Patel R.; Mohammed I.; Bashir M. Head-to-head: Zone 2 vs. Zone 3 frozen elephant trunk. Vessel Plus. 2023, 7, 6. http://dx.doi.org/10.20517/2574-1209.2022.41
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 6 clicks
Cite This Article 6 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.