Global variation in the incidence of new-onset postoperative atrial fibrillation after cardiac and non-cardiac surgery: a systematic review
Abstract
Aim: In the US, postoperative atrial fibrillation (POAF) is the most common complication after cardiac surgery and a frequent complication after non-cardiac surgery, causing excess patient length of stay and costs. After a comprehensive review looking for validated statistically significant data sets, too few data, particularly from outside of the US and Europe, could be found to perform a conclusive analysis, but there is enough data for a well-informed, educated opinion.
Methods: A systematic review analyzing 28 international and US studies of POAF hospital length of stay were identified; from this excess and % excess along with total patient length of stay were calculated, where excess patient length of stay is defined as the difference in post-operative stay between POAF and non-POAF patients in days. Geographic variabilities were calculated using chi-square analyses for US regions and international comparisons for a variety of surgical procedures with POAF.
Results: Geographic variability analyses when corrected for total hospital stay showed a 325% longer excess patient length of stay (days) in the US vs. Europe (3.4 days vs. 0.8 days) for coronary artery bypass grafting (CABG). It also showed a 27.3% longer excess patient length of stay (days) in the US vs. Europe (4.2 days vs. 3.3 days) for lung resections. These were both statistically significant at P < 0.001.
Conclusion: There appear to be substantial variations in POAF-related care practices worldwide. In all practice settings, POAF causes increased patient length of stay. Europeans appear to do better than the US in POAF patients’ length of stay for CABG but not for lung resections. POAF is a worldwide problem where international cooperation in research and development of best practice guidelines would be particularly fruitful.
Keywords
INTRODUCTION
Postoperative atrial fibrillation (POAF) is the most common complication after cardiac surgery with rates up to 65% for certain procedures[1]. In non-cardiac surgeries rates of complication can range from < 0.01% to 50.3%[2]. With 900,000 cardiac procedures performed each year in the US of which a quarter to a third will have POAF, this entity has garnered renewed attention in recent years[3]. Despite the increased attention, there has been little change in overall prevalence over the years with significant variations being reported and an ongoing search for effective prophylactic treatment strategies[4].
Since the early ’70s, research has shown that POAF is associated with an increased hospital stay, morbidity, costs, and long-term outcomes[5]. With prophylaxis in its infancy and treatment only starting after the onset of POAF with unclear guidelines, few resources have been devoted to assessing the associated healthcare impact. To support future research evaluating surgical care patterns of practice, this systematic review compiled published findings on the excessive POAF length of stays observed for both thoracic and non-thoracic procedures.
For POAF patients, there has been large variability in the extra length of stay that was historically documented -- ranging from as little as 0.5 days to as much as 20.3 days[6,7]. Such comparisons ignore, however, different care models and hence may be deceiving. Comparing the total patient length of stay with and without POAF, this systematic review evaluated the regional and international patient length of stay across different surgical procedures to document the variations in POAF care practices; thus, best practices might be identified to serve as a starting point for a worldwide quality improvement effort.
METHODS
For this qualitative content analysis, a PUBMED search was conducted (completed as of June 15, 2021). Each manuscript was assessed for inclusion based upon detailed reports for POAF hospital length of stay for one or more surgical procedures.
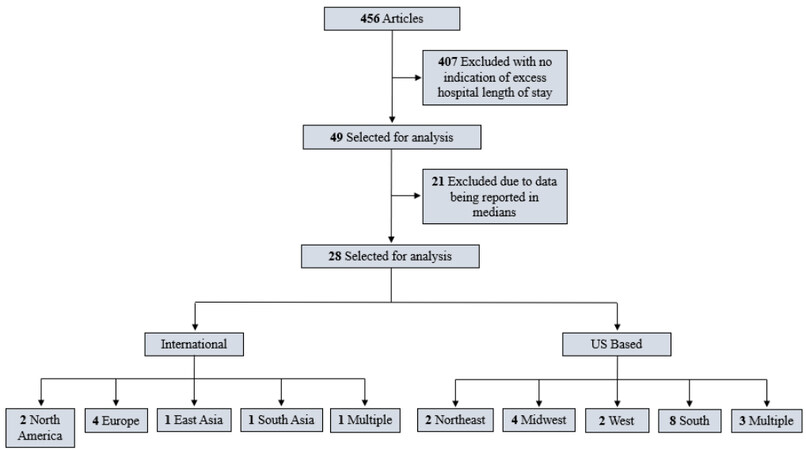
From this search, 456 manuscripts were identified, but only 10.7% (n = 49) included any indication of excess hospital length of stay. Of these 49 manuscripts, 57.1% (n = 28) described the difference in POAF and non-POAF patients’ hospital days using means and 42.8%, (n = 21) reported the length of stay difference using medians. To assure equitable comparisons across different surgical procedures, only the mean differences between POAF versus non-POAF patients’ length of stay were reported. Figure 1 depicts the hierarchy of our exclusion criteria.
US-based geographic data was divided into five regions based on the United States (US) Census Bureau[8]. An additional category was also added, “multiple”, to include studies that encompassed more than one US region.
Legends for US-based Regions
1. Multiple Regions
2. Northeast
3. Midwest
4. South
5. West
Five international regions were also included, and these regions were selected to highlight world-wide geographical differences. The ‘multiple’ region category was created for meta-analyses conducted in more than one region.
Legends for International Regions
1. Multiple Regions
2. North America
3. Europe
4. East Asia
5. South Asia
Included procedures were divided into two categories: thoracic and non-thoracic procedures with 10 and 4 procedure types considered respectively. The categories labeled ‘general’ included more than one procedure under the umbrella categories of either non-cardiac or cardiac surgery.
Legends for Cardiac Procedures
1. General
2. Coronary Bypass Graft (CABG)
3. Off-Pump Coronary Bypass (OPCAB)
4. Atrio-Ventricular Valve (AV Valve)
5. Mitral Valve Repair (MVR)
6. Aortic Arch Repair (AOAR)
Legends for Non-Cardiac Procedures
1. General
2. Thoracotomy
3. Lung Transplant
4. Esophagectomy
5. Lung Resection
6. Abdominal Aortic Repair (AAR)
7. Liver Transplant
8. Hip Replacement
Each manuscript’s findings were reported as either mean or median. Of the 49 manuscripts, 57.1% (n = 28) reported differences in POAF versus non-POAF lengths of stay by comparing means. Using these findings, the POAF versus non-POAF mean findings for length of stay (in days) were compiled and compared between thoracic and non-thoracic procedures and across geographic regions.
The 28 manuscripts were then summarized to identify the POAF-related difference in hospital length of stay. Excess hospital stay was defined as the postoperative hospital stay with atrial fibrillation (days) minus the postoperative hospital stay without atrial fibrillation (days). The study size was also considered along with region and procedure type when evaluating these 28 studies.
Furthermore, due to data scarcity, studies were divided into US versus International regions and by procedure type. For the tabulated regions and procedures, the difference in mean length of stay (in days) and percentage of stay (based in days) due to POAF were reported. For procedures and regions with more than one publication, weighted averages and standard deviations were reported based on the proportion of atrial fibrillation (AF) patients.
Excess days accounted by POAF = (Avg non POAF PLOS - Avg POAF PLOS)
Percent Excess days accounted by POAF = (Excess days accounted by POAF * AF Pts)/(Total Patients)
Although other factors (e.g., differences in other patient risk characteristics) might impact of length of stay (LOS), the assumption was that the reported differences should be primarily attributed to POAF. This assumption afforded simplicity by assuming homogeneity for POAF versus non-POAF patients’ length of stay for the manuscripts analyzed. To evaluate the variability across regions and procedures, chi-square tests were used; a pre-established P-value < 0.05 was used to identify to identify statistically significant differences for the comparisons detailed below:
1. US vs. Europe CABG Total Hospital Stay w/ & w/o POAF
2. US vs. Canada Lung Transplant Total Hospital Stay w/ & w/o POAF
3. US vs. Canada/Europe Lung Resection Total Hospital Stay w/ & w/o POAF
4. US vs. US-South CABG Total Hospital Stay w/ & w/o POAF
5. US vs. US Northeast CABG Total Hospital Stay w/ & w/o POAF
Because of different healthcare systems and care patterns, particularly for the international comparison, the differences in total patient length of stay with and without POAF were used to identify the influence of POAF.
RESULTS
Of the 28 manuscripts analyzed 67.8% (n = 19/28) were based in the United States and 32% (n = 9/28) were conducted internationally, as shown see Tables 1 and 2. The average study’s sample size in the US was 20,042 but skewed heavily by one study evaluating 375 US hospitals with 370,447 patients. In contrast, the average international study’s sample size was 818, with the largest international study’s sample size of 2,852.
Cardiac studies variations in length of stay (international + regional)
| Procedure | Location | Study size | Excess hospital stay* | Total LOS w/ POAF | Total LOS w/o POAF |
| CABG | 24 US Hospitals | 2265 | 2.6 | 12.8 | 10.2 |
| 17 VA Centers | 2103 | 2.9 | 13.2 | 10.3 | |
| Brigham Hospital | 570 | 6.0 | 15.3 | 9.3 | |
| DeBakey VA Medical Center | 1248 | 2.4 | 12.7 | 10.3 | |
| Washington Hospital Center | 969 | 3.0 | 9.0 | 6.0 | |
| Texas Heart Institute | 6475 | 4.0 | 14.0 | 10.0 | |
| US, Italy, Argentina | 1462 | 1.3 | 11.3 | 10 | |
| Thoracic & Cardiovascular Surgery Center Istanbul (Turkey) | 756 | 0.81 | 8.66 | 7.85 | |
| Amrita Institute of Medical Sciences (India) | 748 | 4.99 | 15.8 | 10.81 | |
| Mitral valve repair | University of North Carolina | 5613 | 0.5 | 4.9 | 4.5 |
| AOAR | National Cardiovascular Center (Japan) | 459 | 13.0 | 48 | 35 |
Non-cardiac studies variations in length of stay (international + regional)
| Procedure | Location | Study size | Excess hospital stay* | Total LOS w/ POAF | Total LOS w/o POAF |
| Lung transplant | University of Texas Southwestern | 131 | 8.43 | 25.52 | 17.09 |
| Duke Hospital | 200 | 14.9 | 32.4 | 17.5 | |
| Centre Hospitalier de l’Universite de Montreal (Canada) | 224 | 20.3 | 51.5 | 31.2 | |
| Lung resection | Portland, Oregon | 1036 | 4.2 | 10.4 | 6.2 |
| Ottawa Hospital (Canada) | 363 | 3.6 | 10.5 | 6.9 | |
| Guy’s Hospital (UK) | 43 | 4.02 | 10.8 | 6.78 | |
| Varese University Hospital (Italy) | 454 | 3.1 | 15.3 | 12.2 | |
| General thoracic & non-thoracic | 375 US Hospitals | 370,447 | 8.1 | 15.0 | 6.9 |
| General thoracic | University of Texas | 2588 | 8.4 | 16.6 | 8.2 |
| General non-thoracic | DeBakey VA Medical Center | 354 | 8.3 | 35.0 | 26.7 |
| Esophagectomy | Mayo Clinic Arizona | 121 | 2.8 | 13.4 | 10.6 |
| Medical College of Wisconsin | 71 | 1.6 | 15.1 | 13.5 | |
| Creighton University SOM | 192 | 5.0 | 19.0 | 14.0 | |
| Thoracotomy | Memorial Sloan-Kettering | 527 | 9.0 | 17.0 | 9.0 |
| Hip replacement | Università Di Firenze (Italy) | 2852 | 5.3 | 19.7 | 14.4 |
| AAR | Loyola University Chicago | 4462 | 8.1 | 18.7 | 8.6 |
| Liver transplant | Indiana University | 1011 | 9.0 | 18.0 | 9.0 |
Table 1 breaks each of the cardiac studies used in this manuscript by procedure type and location. Included are study size (# patients), excess hospital stay (days), and total LOS by POAF and non-POAF (days).
Table 2 breaks down non-cardiac studies in the same way as stated above. For US studies, the mean total LOS across all thoracic procedures was 15.8 ± 6.6 days for POAF patients and 10.1 ± 3.7 days for non-POAF patients. Additionally, the US-based mean total LOS across all non-thoracic procedures was 26.5 ± 8.5 for POAF patients and 17.9 ± 8.9 days for non-POAF patients. For international studies, the mean total length of stay across all thoracic procedures was 17.7 ± 14.0 days for POAF patients and 12.2 ± 8.0 days for non-POAF patients. Moreover, the international mean total LOS across all non-thoracic procedures was 33.9 ± 14.2 days for POAF patients and 24.7 ± 10.3 days for non-POAF patients.
Table 3 attempts to further explain the trends seen in Tables 1 and 2 by identifying the impact POAF has on specific procedures through excess LOS displayed in days and percentages. In the US, the POAF-based impact upon LOS was ranked as follows: lung transplant (468.27%), thoracotomy (119.92%), esophagectomy (95.89%), CABG (69.3%), lung resection (45.81%), mitral valve repair (25.33%). There were only 2 non-thoracic US procedures and they ranked as follows: liver transplant (90.80%) and abdominal aortic repair (24.67%).
Cardiac + non-cardiac procedures postoperative length of stay geographic variations
| International | US | |||||
| n | Excess AFIB Mean PLOS* | % Excess AFIB Mean PLOS | Excess AFIB Mean PLOS* | % Excess AFIB Mean PLOS | ||
| General non-thoracic & thoracic | 370447 | - | - | 8.1 | 23.96% | |
| Non-cardiac | General thoracic | 2588 | - | - | 8.4 | 103.54% |
| General non-thoracic | 2942 | - | - | 8.3 | 70.34% | |
| Thoracotomy | 527 | - | - | 8.0 | 119.92% | |
| Lung resection (SD) | 2230 | 3.3 (0.5) | 39.13% (0.1) | 4.2 | 45.81% | |
| Lung transplant (SD) | 555 | 20.3 | 589.06% | 12.5 (4.6) | 468.27% (2.0) | |
| Esophagectomy | 192 | - | - | 3.2 (1.7) | 95.89% (0.3) | |
| AAR | 4462 | - | - | 10.1 | 24.67% | |
| Liver transplant | 1011 | - | - | 9 | 90.80% | |
| Hip replacement | 2852 | 5.3 | 19.33% | - | - | |
| Cardiac | AOAR | 459 | 13 | 685.40% | - | - |
| Mitral valve repair | 5613 | - | - | 0.4 | 25.33% | |
| CABG (SD) | 16,596 | 1.8 (2.3) | 45.93% (0.3) | 3.4 (1.4) | 69.3% (0.6) | |
Table 4 exhibits the POAF-based variations across geographical regions using total hospital stay. Compared to non-POAF patients, POAF patients had longer lengths of stay across all regional comparisons.
Regional postoperative length of stay variations by procedure type
| Total POAF | Total non-POAF | Excess hospital stay | P value* | |
| US CABG | 13.2 ± 2.1 (n = 36,563) | 9.8 ± 1.7 (n = 106,366) | 3.4 (n = 142,929) | < 0.00001 |
| Europe CABG | 8.7 (n = 1394) | 7.9 (n = 4671) | 0.8 (n = 6065) | |
| US Lng TX | 29.8 ± 4.9 (n = 3701) | 17.3 ± 0.3 (n = 3588) | 12.5 (n = 7289) | < 0.00001 |
| Canadian Lng TX | 51.5 (n = 3348) | 31.2 (n = 4961) | 20.3 (n = 8309) | |
| US Lng resection | 10.4 (n = 1175) | 6.2 (n = 5723) | 4.2 (n = 6898) | < 0.00001 |
| Canadian/European Lng resection | 12.2 ± 2.7 (n = 1604) | 8.9 ± 3.1 (n = 9462) | 3.3 (n = 11,066) | |
| South US CABG | 13.1 ± 2.6 (n = 18,501) | 9.6 ± 2.4 (n = 70,028) | 3.5 (n = 88,529) | < 0.00001 |
| General US CABG | 13.0 ± 0.3 (n = 15,171) | 10.2 ± 0.1 (n = 32,795) | 2.8 (n = 47,966) | |
| Northeast US CABG | 15.3 (n = 2892) | 9.3 (n = 3543) | 6.0 (n = 6435) | < 0.00001 |
| General US CABG | 13.0 ± 0.3 (n = 15,171) | 10.2 ± 0.1 (n = 32,795) | 2.8 (n = 47,966) |
Comparing US vs. Europe CABG procedures. the US CABG patients had dramatically increased LOS(P < 0.00001). Evaluating the POAF excessive stay (in days), the US-based POAF patients stayed an additional 3.4 days on average as compared to the European POAF patients staying an additional 0.8 days.
The second comparison made for was US vs. Canada lung transplant procedures. POAF’s impact when accounting for total hospital stay demonstrated a statistically significant increase in LOS as compared to Canada (P < 0.00001). Canada’s POAF-related excess in hospital stay was 20.3 days vs. the US, which was 12.5 days.
The third and last international comparison made was US vs. Canada/Europe lung resection procedures. POAF’s impact upon total hospital stay demonstrated a statistically significant decrease in LOS when compared to the US (P < 0.00001). US POAF-related excess in hospital stay was 4.2 days vs. Canada/Europe, which was 3.3 days.
The fourth comparison was between US-South vs. General US CABG procedures. POAF’s impact when accounting for the total hospital stay demonstrated a statistically significant increase in POAF in the South (P < 0.00001). The South’s excess hospital stay was 3.5 days vs. General US, which was 2.8 days.
The fifth and last comparison between US regions is US Northeast vs. General US CABG procedures. POAF’s impact when accounting for the total hospital stay demonstrated a statistically significant increase in POAF in the Northeast (P < 0.00001). The Northeast’s POAF-related excess in hospital stay was 6.0 days vs. General US, which was 2.8 days.
In summary, there was substantial heterogeneity within the US as to a CABG POAF-related impact. When examined regionally, CABG procedures performed at institutions located in both the South and Northeast had prolonged POAF patients’ LOS as compared to the rest of the country [Table 4].
DISCUSSION
Summarizing 28 publications, this novel systematic review provides a world-wide assessment of the POAF impact upon different surgical procedures’ length of stay. In all cases, substantial variability was found when comparing POAF versus non-POAF patients’ differences in length of stay across procedures and geographic regions.
This type of study, however, inherently suffers from many weaknesses regarding the data. Most reports included are from single institutions. These are often regional referral centers that do not necessarily represent the general care provided in the wider geographic region. There is also a tendency to compare US data on geography when a more representative comparison could have been made between health systems if a more diversified data set were available.
Further, a comparison of these reports is hampered by a very large publication time span stretching over decades. This is mitigated by the fact that the incidence of POAF has scarcely changed over the last 50 years. The studies included tended to be from institutions with larger volumes which we know affects the outcome. Hannan et al. examined CABG procedures in the state of New York to determine if procedural volume affected risk-adjusted mortality rates. He concluded that higher volume does indeed predict a reduction in mortality rates[36]. The best-documented procedure in this study is CABG which again is likely volume-related: the scientific registry of transplant recipients shows only 73 centers that perform lung transplants in the US as of 2021[37]. In contrast, in 2003, health affairs showed that 1,069 hospitals performed CABG procedures in the US[38]. Every year in the US, approximately 8000 liver transplants and 2000 lung transplants are performed[39,40]. This is in contrast to the approximately 500,000 CABG procedures performed in the US each year, one of the most commonly occurring procedures in general[41]. Thus, the finding that POAF in Europe is associated with fewer in-hospital days than in the US has probably the most validity, a finding further underpinned by a significant difference in total hospital days for that procedure.
Another interesting finding in our research is how varied the impact of POAF depends on the procedure. When POAF occurs after a CABG, only an increase of 3.4 and 0.8 days occurred in the US and internationally, respectively. In contrast, lung transplant and lung resection had much larger impacts on their LOS, with 12.5 and 4.2 increased days in the US, respectively. This begs the question if cardiac procedures have a decreased LOS impact when POAF occurs when compared to non-cardiac procedures. This is an area where further research could be devoted to unraveling the causes, such as if hospital POAF treatments were different between cardiac & non-cardiac procedures.
There also needs to be consideration as to whether differences between POAF versus non-POAF patients’ length of stay was an accurate and reliable comparison given the lack of adjustments that could be performed addressing hospital burden or variations in patient comorbidity. Gillinov et al. surprisingly showed no POAF -related changes in LOS or other complications[42]. As this study assumed that POAF was the driving force behind the LOS differences observed, many other patient risk factors (e.g., patients’ age, race, ethnicity, socioeconomic status, etc.) and surgery-specific technical details (e.g., robotic, off-pump, etc.) may also have impacted these reported LOS. Given these limitations, additional research appears warranted to rigorously compare risk-adjusted LOS between POAF and non-POAF patients across surgical procedures and geographic regions, as well as to evaluate for trends over time.
In conclusion, this systematic review has documented that POAF is not just a cardiac surgical problem but affects all types of operations with decreasing frequency the further away from the heart they take place. Moreover, it is a worldwide problem with a wide variability of the POAF impact upon patients’ length of stay. National, regional, and local health care systems have different approaches arguably because of a lack of consensus as to best practices. This is fertile ground for international collaboration especially since the economic savings are enormous.
DECLARATIONS
Authors’ contributionsSubstantial contributions to this study’s conceptualization and qualitative design: Pardo D, Bilfinger T, Shroyer AL
Coordinated the literature review, captured the study data, performed the preliminary analysis, and provided summary reports describing this study’s findings: Pardo D
Verified sample of data captured and guided the analysis: Shroyer AL, Bilfinger T
Prepared the first manuscript draft: Pardo D, Bilfinger T
Revised the manuscript substantively and provided final manuscript approval: Pardo D, Bilfinger T, Shroyer AL
Availability of data and materialsThe data extracted for this study have been made available for independent review Supplementary appendix.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethics approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Rostagno C, La Meir M, Gelsomino S, et al. Atrial fibrillation after cardiac surgery: incidence, risk factors, and economic burden. J Cardiothorac Vasc Anesth 2010;24:952-8.
2. McIntyre WF, Vadakken ME, Rai AS, et al. Incidence and recurrence of new-onset atrial fibrillation detected during hospitalization for non-cardiac surgery: a systematic review and meta-analysis. Can J Anaesth 2021;68:1045-56.
3. Research iData. How many cardiac surgeries are performed each year? - New study by iData research [Internet]. IData Res. 2021 [cited 2021 Oct 11]. Available from: https://idataresearch.com/over-900000-cardiac-surgeries-performed-every-year-in-the-united-states/ [Last accessed on 8 Jun 2022].
4. Almassi GH, Wagner TH, Carr B, et al. VA #517 Randomized On/Off Bypass (ROOBY) Study Group. Postoperative atrial fibrillation impacts on costs and one-year clinical outcomes: the Veterans Affairs Randomized On/Off Bypass Trial. Ann Thorac Surg 2015;99:109-14.
5. Almassi GH, Schowalter T, Nicolosi AC, et al. Atrial fibrillation after cardiac surgery: a major morbid event? Ann Surg 1997;226:501-13.
6. Arora S, Vemulapalli S, Stebbins A, et al. The prevalence and impact of atrial fibrillation on 1-year outcomes in patients undergoing transcatheter mitral valve repair: results from the society of thoracic surgeons/American college of cardiology transcatheter valve therapy registry. JACC Cardiovasc Interv 2019;12:569-78.
7. Henri C, Giraldeau G, Dorais M, et al. Atrial fibrillation after pulmonary transplantation: incidence, impact on mortality, treatment effectiveness, and risk factors. Circ Arrhythm Electrophysiol 2012;5:61-7.
8. Bureau UC. 2010 Census Regions and Divisions of the United States [Internet]. Census.gov. [cited 2021 Oct 11]. Available from: https://www.census.gov/geographies/reference-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html [Last accessed on 8 Jun 2022].
9. Bhave PD, Goldman LE, Vittinghoff E, Maselli J, Auerbach A. Incidence, predictors, and outcomes associated with postoperative atrial fibrillation after major noncardiac surgery. Am Heart J 2012;164:918-24.
10. Mathew JP. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. JAMA 1996;276:300.
11. Burrage PS, Low YH, Campbell NG, O’Brien B. New-onset atrial fibrillation in adult patients after cardiac surgery. Curr Anesthesiol Rep 2019;9:174-93.
12. Aranki SF, Shaw DP, Adams DH, et al. Predictors of atrial fibrillation after coronary artery surgery. Current trends and impact on hospital resources. Circulation 1996;94:390-7.
13. Vaporciyan AA, Correa AM, Rice DC, et al. Risk factors associated with atrial fibrillation after noncardiac thoracic surgery: analysis of 2588 patients. J Thorac Cardiovasc Surg 2004;127:779-86.
14. Omer S, Cornwell LD, Bakshi A, et al. Incidence, predictors, and impact of postoperative atrial fibrillation after coronary artery bypass grafting in military veterans. Tex Heart Inst J 2016;43:397-403.
15. Stamou SC, Dangas G, Hill PC, et al. Atrial fibrillation after beating heart surgery. The American Journal of Cardiology 2000;86:64-7.
16. Villareal RP, Hariharan R, Liu BC, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol 2004;43:742-8.
17. Raghavan D, Gao A, Ahn C, et al. Contemporary analysis of incidence of post-operative atrial fibrillation, its predictors, and association with clinical outcomes in lung transplantation. J Heart Lung Transplant 2015;34:563-70.
18. Nielsen TD, Bahnson T, Davis RD, Palmer SM. Atrial fibrillation after pulmonary transplant. Chest 2004;126:496-500.
19. Day RW, Jaroszewski D, Chang YH, et al. Incidence and impact of postoperative atrial fibrillation after minimally invasive esophagectomy. Dis Esophagus 2016;29:583-8.
20. Colwell EM, Encarnacion CO, Rein LE, et al. Atrial fibrillation after transhiatal esophagectomy with transcervical endoscopic esophageal mobilization: one institution’s experience. J Cardiothorac Surg 2018;13:73.
21. Blanco BA, Kothari AN, Halandras PM, et al. Transient atrial fibrillation after open abdominal aortic revascularization surgery is associated with increased length of stay, mortality, and readmission rates. J Vasc Surg 2017;66:413-22.
22. Rachwan RJ, Kutkut I, Hathaway TJ, et al. Postoperative atrial fibrillation and flutter in liver transplantation: an important predictor of early and late morbidity and mortality. Liver Transpl 2020;26:34-44.
23. Amar D, Zhang H, Leung DH, Roistacher N, Kadish AH. Older age is the strongest predictor of postoperative atrial fibrillation. Anesthesiology 2002;96:352-6.
24. Kotova S, Wang M, Lothrop K, Grunkemeier G, Merry HE, Handy JR. CHADS2 score predicts postoperative atrial fibrillation in patients undergoing elective pulmonary lobectomy. Ann Thorac Surg 2017;103:1566-72.
25. Burris JM, Subramanian A, Sansgiry S, Palacio CH, Bakaeen FG, Awad SS. Perioperative atrial arrhythmias in noncardiothoracic patients: a review of risk factors and treatment strategies in the veteran population. Am J Surg 2010;200:601-5.
26. Lohani KR, Nandipati KC, Rollins SE, et al. Transthoracic approach is associated with increased incidence of atrial fibrillation after esophageal resection. Surg Endosc 2015;29:2039-45.
27. Akintoye E, Sellke F, Marchioli R, Tavazzi L, Mozaffarian D. Factors associated with postoperative atrial fibrillation and other adverse events after cardiac surgery. J Thorac Cardiovasc Surg 2018;155:242-251.e10.
28. Ivanovic J, Maziak DE, Ramzan S, et al. Incidence, severity and perioperative risk factors for atrial fibrillation following pulmonary resection. Interact Cardiovasc Thorac Surg 2014;18:340-6.
29. Vural Ü, Ağlar AA. What is the role of metabolic syndrome and obesity for postoperative atrial fibrillation after coronary bypass grafting? BMC Cardiovasc Disord 2019;19:147.
30. Garner M, Routledge T, King JE, et al. New-onset atrial fibrillation after anatomic lung resection: predictive factors, treatment and follow-up in a UK thoracic centre. Interact Cardiovasc Thorac Surg 2017;24:260-4.
31. Imperatori A, Mariscalco G, Riganti G, Rotolo N, Conti V, Dominioni L. Atrial fibrillation after pulmonary lobectomy for lung cancer affects long-term survival in a prospective single-center study. J Cardiothorac Surg 2012;7:4.
32. Rostagno C, Cartei A, Rubbieri G, et al. Postoperative atrial fibrillation is related to a worse outcome in patients undergoing surgery for hip fracture. Intern Emerg Med 2021;16:333-8.
33. Matsuura K, Ogino H, Matsuda H, et al. Prediction and incidence of atrial fibrillation after aortic arch repair. Ann Thorac Surg 2006;81:514-8.
34. Ghurram A, Krishna N, Bhaskaran R, Kumaraswamy N, Jayant A, Varma PK. Patients who develop post-operative atrial fibrillation have reduced survival after off-pump coronary artery bypass grafting. Indian J Thorac Cardiovasc Surg 2020;36:6-13.
35. Social Science Statistics [Internet]. [cited 2021 Nov 11]. Available from: https://www.socscistatistics.com/ [Last accessed on 8 Jun 2022].
36. Hannan EL, Wu C, Ryan TJ, et al. Do hospitals and surgeons with higher coronary artery bypass graft surgery volumes still have lower risk-adjusted mortality rates? Circulation 2003;108:795-801.
37. Transplant Centers [Internet]. [cited 2021 Nov 17]. Available from: https://www.srtr.org/transplant-centers/?&organ=lung&recipientType=adult&sort=volume [Last accessed on 8 Jun 2022].
38. Wilson CT, Fisher ES, Welch HG, Siewers AE, Lucas FL. U.S. trends in CABG hospital volume: the effect of adding cardiac surgery programs. Health Aff (Millwood) 2007;26:162-8.
39. Lung Transplant | Michigan Medicine [Internet]. [cited 2021 Nov 15]. Available from: https://www.uofmhealth.org/conditions-treatments/transplant/adult-lung-transplant [Last accessed on 8 Jun 2022].
40. The Facts About Liver Transplant: Survival Rates, Statistics, and More [Internet]. Healthline. 2016 [cited 2021 Nov 15]. Available from: https://www.healthline.com/health/liver-transplant-survival [Last accessed on 8 Jun 2022].
41. Coronary artery bypass grafting - HonorHealth [Internet]. [cited 2021 Nov 15]. Available from: https://www.honorhealth.com/medical-services/cardiac-care/treatment-options/coronary-artery-bypass-grafting [Last accessed on 8 Jun 2022].
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Pardo D, Shroyer AL, Bilfinger TV. Global variation in the incidence of new-onset postoperative atrial fibrillation after cardiac and non-cardiac surgery: a systematic review. Vessel Plus 2022;6:50. http://dx.doi.org/10.20517/2574-1209.2021.146
AMA Style
Pardo D, Shroyer AL, Bilfinger TV. Global variation in the incidence of new-onset postoperative atrial fibrillation after cardiac and non-cardiac surgery: a systematic review. Vessel Plus. 2022; 6: 50. http://dx.doi.org/10.20517/2574-1209.2021.146
Chicago/Turabian Style
Pardo, Daniel, A. Laurie Shroyer, Thomas V. Bilfinger. 2022. "Global variation in the incidence of new-onset postoperative atrial fibrillation after cardiac and non-cardiac surgery: a systematic review" Vessel Plus. 6: 50. http://dx.doi.org/10.20517/2574-1209.2021.146
ACS Style
Pardo, D.; Shroyer AL.; Bilfinger TV. Global variation in the incidence of new-onset postoperative atrial fibrillation after cardiac and non-cardiac surgery: a systematic review. Vessel Plus. 2022, 6, 50. http://dx.doi.org/10.20517/2574-1209.2021.146
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 6 clicks
Cite This Article 6 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.