Management of anticoagulant treatment in patients who need non-cardiac surgery
Abstract
The periprocedural management of anticoagulation in patients who require non-cardiac surgery is a common clinical problem due to the aging of the population associated with both an increase in the use of anticoagulants and a higher need for surgery. If surgery is needed in a patient on anticoagulant therapy, regardless of the drug used, it is necessary to consider the urgency of the surgical procedure and the balance between the thromboembolic risk related to the discontinuation of therapy and the hemorrhagic risk related to the surgical procedure itself. Finally, a topic still much discussed that derives from the combined evaluation of these factors is the possible indication of a bridge therapy (“bridging anticoagulation”) to limit the thromboembolic risk related to the discontinuation of treatment. The different strategies in patients under antivitamin K and direct oral anticoagulants are reviewed.
Keywords
INTRODUCTION
As the population ages, the already high number of patients taking oral anticoagulant therapy is inevitably expected to increase. At the same time, in subjects over 65 years of age, the probability of undergoing surgery is constantly growing. It has been calculated that in the first two years following the start of anticoagulant treatment, about a quarter of patients require discontinuation of therapy for a scheduled intervention[1,2].
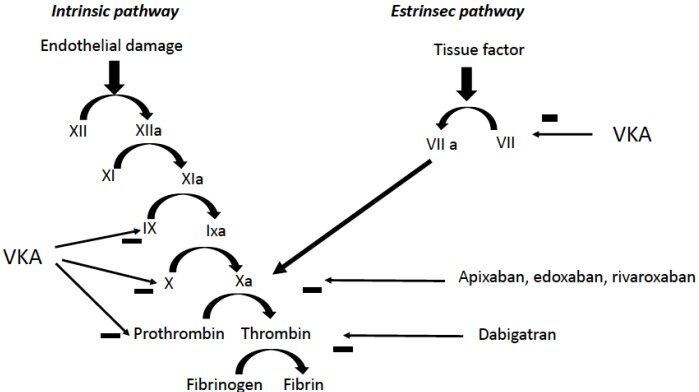
Over the last decade, direct anticoagulants have largely replaced drugs with antivitamin K action, which nevertheless retain well-defined indications. The anticoagulant action of dicoumarols is linked to the ability to interfere with epoxide reductase, which allows the conversion of vitamin K into its 2.3 epoxide [Figure 1]. This prevents the gamma-carboxylation process of glutamate residues of factors II, VII, IX, and X[3,4]. Vitamin K is also essential in the synthesis of C and S proteins, endowed with anticoagulant action. The short half-life of protein C means that in the first phase of treatment with warfarin, a pro-coagulant effect may be observed, which is why treatment with heparin is necessary in the induction phase of treatment with vitamin K antagonists.
Numerous studies have shown a therapeutic efficacy of direct anticoagulants comparable to warfarin and, on average, a lower hemorrhagic risk[5,6]. They also have the considerable advantage of not requiring periodic monitoring [Table 1].
Main difference between direct anticoagulants and antivitamin K
| Antivitamin K | Direct anticoagulants | |
| Onset of action | Long (days) | Short (2-3 h) |
| Duration of action | Long | Brief |
| Food interference | Yes | Limited (rivaroxaban should be taken after a meal) |
| Drug interactions | Yes | Limited |
| Antidote | Yes | Iduracizumab for dabigatran, Andexanet for Xa inhibitors § |
| Renal excretion | No | Yes, essentially for dabigatran |
| Need for monitoring | Yes | No |
If surgery is needed in a patient on anticoagulant therapy, regardless of the drug used, it is necessary to consider the urgency of the surgical procedure to which the patient must be subjected and the balance between the thromboembolic risk related to the discontinuation of therapy and the hemorrhagic risk related to the surgical procedure itself. Finally, a topic still much discussed that derives from the combined evaluation of the factors mentioned is the possible indication of a bridge therapy (“bridging anticoagulation”) to limit the thromboembolic risk related to the discontinuation of treatment, but which is inevitably associated with an increased hemorrhagic risk related to the surgical procedure.
Stratification of thromboembolic risk
Risk stratification is reported for the three main indications for anticoagulant therapy [Table 2]. In patients at high thromboembolic risk at the time of discontinuation of anticoagulant therapy, treatment with heparin, unfractionated or low molecular weight, as a bridge therapy may be indicated to limit the risks of thrombotic complications.
Stratified risk of thromboembolism in different clinical settings (modified from[2])
| Valve prosthesis | Non valvular AF | Venous thromboembolism | |
| High | Mitral valve mechanic prosthesis Ball or disk aortic prosthesis CVA/TIA in the previous 6 months | CHADS2 score 5 or 6. CHA2DS2VASc? CVA/TIA in the previous 3 months Rheumatic valve disease | Episode in the previous 3 months Severe thrombophilia |
| Intermediate | Two-hemidisk aortic valve with additional risk factors | CHADS2 score 3 or 4 CHA2DS2VASc? No CVA/TIA | Episode in the previous 4-12 months Not severe thrombophilia§ Recurring episodes Neoplasms Recurring episodes Neoplasms |
| Low | Two-hemidisk aortic valve with no additional risk factors | CHADS2 score 2 or less CHA2DS2VASc? No CVA/TIA | Episode occurred > 12 months prior No additional risk factors |
The introduction of a more accurate thromboembolic risk scheme, for example, CHA2DS2VASc, does not seem to offer substantial additional elements. It is therefore still unresolved, for patients with NVAF, whether the indication for a bridge therapy is useful to consider an absolute cut-off value or, alternatively, to consider at high risk of thrombotic events, essentially those patients who have had a previous cerebral or systemic embolic event.
Estimation of bleeding risk
In the assessment of bleeding risk, individual factors (age, renal function, recent ischemic or hemorrhagic events, concomitant treatment with antiplatelet agents, thrombocytopenia, and liver disease) and factors related to the procedure (type of procedure, possibility to obtain adequate hemostasis, and the district involved by surgery) should be considered [Table 3]. The different patterns reported by the guidelines or consensus conferences provide a distinction in procedures with negligible, low-moderate, and high risk of bleeding[7].
Stratification of hemorrhagic risk (modified[7])
| Negligible risk |
| Dental interventions (extraction of 1-3 teeth, periodontal surgery, incision of abscesses, or implantology) Ophthalmology (cataract surgery or glaucoma) |
| Non-interventional endoscopic procedures |
| Superficial surgery (e.g., incision of abscesses or removal of small skin lesions) |
| Low risk |
| Endoscopic procedures with biopsy |
| Bladder and prostatic biopsies |
| Non-coronary angiography |
| Electrophysiological study or transcatheter ablation in the right chambers |
| Pacemaker or defibrillator implant (if anatomy is not complex) |
| High risk |
| Transcatheter ablation in the left heart chambers |
| Spinal or epidural anesthesia or lumbar puncture |
| Thoracic, abdominal, or orthopedic major surgery |
| Hepatic or renal biopsy |
| Transurethral resection of the prostate |
| Lithotripsy with wave shock |
Non-complex dental surgery, most ophthalmology and dermatological surgery, and endoscopic procedures that do not require biopsy can be performed without any interruption of anticoagulant therapy. In patients with indications for surgery, in whom the hemorrhagic risk of the procedure is incompatible with the maintenance of anticoagulation, this should be discontinued. The time of discontinuation is related to the half-life of the anticoagulant drug.
Surgical timing
In relation to the timing of surgery, different strategies should be considered in elective procedures, for which there are consolidated indications in comparison to emergency (need to intervene within minutes), urgency (need to intervene within hours), and time-dependent procedures (beyond 24 h). Time-dependent procedures may be considered those interventions for which the results are strictly influenced by the timing of the intervention. A typical example, very frequent considering the age group, is the surgery for hip fracture in which the outcome in terms of both survival and functional recovery is closely related to the precocity of the intervention (within 48 h of trauma).
WARFARIN
Elective surgery
Warfarin discontinuation should take place 5-7 days before surgery. Considering the pharmacokinetic characteristics of warfarin, on the fifth day after discontinuation, the residual pharmacological action is approximately 3%. Depending on the individual embolic risk, a “bridge therapy” through administration of short half-life anticoagulants, unfractionated heparin (UFH), or low molecular weight heparin (LMWH) may or may not be considered.
In the past, intravenous infusion of UFH has been the most widely used solution for anticoagulation bridging; however, due to poor handling, it can currently be found due to its short half-life and the possibility of antagonism with the administration of protamine sulfate indication in surgical procedures characterized by high hemorrhagic risk, such as neurosurgical interventions, in the case of renal failure or recent or active bleeding. Currently, for “bridge therapy”, the use of LWMH is preferred at a dose of about 70%-80% of the full anticoagulant dose[8]. Although it is advisable to start treatment when International Normalised Ratio (INR) values fall below the therapeutic range, as daily monitoring is not always possible, it is reasonable to start heparin treatment approximately two days after discontinuation of oral anticoagulant therapy. The last dose of LMWH should be 20-25 h away from the procedure, i.e., a period of time open to about five times the elimination half-life of the drug, so that at the time of surgery, there is no residual anticoagulant effect[9,10].
The results of recent studies, however, clearly show that bridge therapy is accompanied by a significant increase in the risk of postoperative bleeding, while no significant protection is observed in the reduction of thromboembolic events, whose incidence is negligible[11]. “Bridge therapy” appears at the moment not indicated as a standard procedure in patients on anticoagulant treatment who must undergo surgery and must be limited to patients with a very high thromboembolic risk (mechanical valve prostheses in the mitral position or recent cerebrovascular or pulmonary thromboembolic event). LMWH at deep vein thrombosis prophylaxis dose should be considered, where necessary, for all other patients[11]. Resumption of warfarin therapy may be considered 24-48 h after the surgical procedure.
Emergency surgery-time-dependent
In patients who need to undergo emergency or strictly time-dependent surgery, such as the treatment of fractures of the proximal third of the femur, rapid restoration of hemostatic function is necessary. Discontinuation of warfarin and administration of vitamin K (1.0-2.5 mg intravenously or 5-10 mg orally) are sufficient to normalize INR within 24-48 h[12]. In patients who require emergency intervention, the administration of coagulation factor concentrates is indicated. For AVKs, the four-factor prothrombin complex concentrates (PCC) dose [administration of four-factor non-activated PCC (CONFIDEX®) may be considered in the case of very high INR values above 4.0] depending on the INR values and the patient’s weight [Table 4][13].
Median dosage of PCC in relation to baseline INR and weight
| INR | PCC dose (KedcomR) | PCC (ConfidexR)§ |
| < 2.0 2-3 3-4 > 4 | 20 UI/kg 30 UI/kg 40 UI/kg 50 UI/kg | |
| 2-3.9 4-6 > 6 | 25UI f IX/kg-1 mL/kg 35UI f IX/kg-1.4 mL/kg 50UI f IX/kg-2 mL/kg |
The administration of vitamin K is especially useful in the case of time-dependent intervention, such as in patients with hip fractures[14]. Several treatment regimens have been proposed both by route of administration, per os or i.v., and by dosage (2.5 or 10 mg)[15]. Oral administration may be preferable, leading in 100% of cases to INR values before surgery < 1.7, in patients with INR values < 3.0, without ongoing bleeding, and in which surgery can be deferred by 24-36 h.
DIRECT ANTICOAGULANTS
Elective surgery
The patient who needs an elective surgical procedure should discontinue treatment with direct anticoagulants. For discontinuation of therapy, several factors should be considered: renal function (creatinine clearance, according to Cockcroft-Gault, although with several limits, is the most frequently used method to evaluate kidney function), the type of drug taken, the interval from the last administration, single or bi-administration, the hemorrhagic risk related to the surgical procedure, and the thromboembolic risk of each patient.
In the case of surgical interventions characterized by a negligible bleeding risk, such as dental interventions or superficial surgery procedures, the last dose of the drug should be taken approximately 18-24 h before surgery for apixaban, rivaroxaban, and edoxaban[16], while the time of withdrawal varies in relation to renal function for dabigatran [Table 5]. If the bleeding risk of the procedure is not negligible but is still low, as in the case of bladder and prostate biopsies or non-coronary angiography, discontinuation of therapy 24 h before is recommended if renal function is normal[17]. If the surgery is characterized by a high bleeding risk, e.g., thoracic, abdominal, or major orthopedic surgery procedures, anticoagulant therapy with apixaban, rivaroxaban, and edoxaban should be discontinued 48 h before surgery. Dabigatran discontinuation times still need to be evaluated on renal function.
Timing of DOACs withdrawal in relation to kidney function and procedural risk of bleeding
| Creatinine clearance | Intervention at low risk of bleeding (< 2% risk within 48 h) | Intervention at high risk of bleeding (2-4% risk within 48 h) |
| Dabigatran | ||
| > 80 mL/min | 24 h | 48 h |
| 50-80 mL/min | 36 h | 72 h |
| 30-50 mL/min | 48 h | 96 h |
| Apixaban, edoxaban, rivaroxaban | ||
| > 80 mL/min | 24 h | 48 h |
| 50-80 mL/min | 24 h | 48 h |
| 30-50 mL/min | 24 h | 48 h |
| 15-30 mL/min | 36 h | 48 h |
Recent data show that in about 20% of patients, a concentration of drugs in the plasma still able to exert an anticoagulant action may be detected more than 48 h after the last intake of a direct anticoagulant, an effect more frequently observed with apixaban. This finding has called into question the safety of the adoption of rigid suspension schemes when neuraxial anesthesia is hypothesized[18].
After surgery in which complete hemostasis could be achieved, direct anticoagulants can generally be resumed 6-8 h after surgery. However, resuming the full anticoagulation dose within the first 48-72 h after most of the thoracic or abdominal procedures may carry a risk of bleeding that outweighs the risk of AF-related embolism. In these cases, postoperative thromboprophylaxis with LMWH in prophylaxis dose 6-8 h after surgery and delay of therapeutic anticoagulation, postponing the restart of direct oral anticoagulants (DOACs) by ≥ 48-72 h, can be considered.
Emergency surgery-time-dependent
Given their short half-life, in a patient with preserved renal function, reduction of the anticoagulant effect occurs relatively quickly from the last intake; for this reason, a waiting strategy accompanied by supportive therapy is considered sufficient if the intervention can be postponed by at least 12-24 h from the last administration. The reversal of anticoagulant activity should instead be considered in conditions of emergency (minutes) or urgency (hours). Before any treatment, the coagulation status of the patient (PT, aPTT, anti-FXa dosage, dTT/ECA, etc.) should be evaluated. Although in an emergency situation, the indication for the use of specific antidotes and/or pro-hemostatic factors is regulated by the clinical presentation of the patient, the results of these initial tests may have important implications for further treatment during the following hours since an excessive prothrombotic state as well as an insufficient reversal may be observed, both needing correction. Recently, it has also been shown that the evaluation of plasma levels of DOAC may be useful in interpreting the anticoagulation state and the residual effects of DOACs[18].
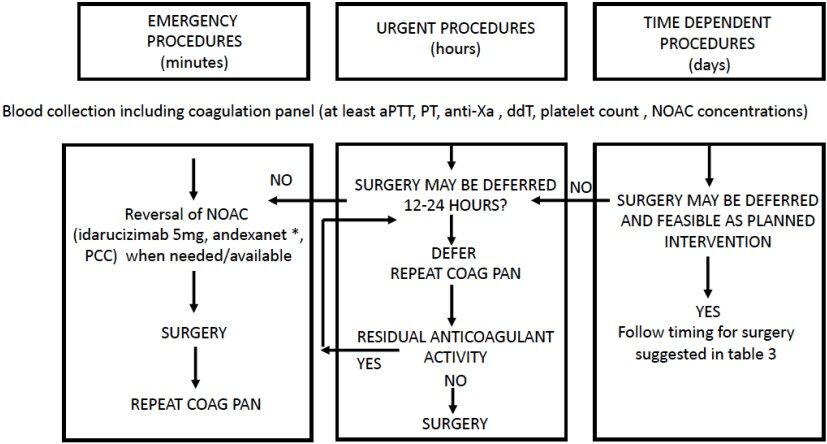
The recent EHRA (European Heart Rhythm Association) guidelines provide an algorithm [Figure 2] for the management of anticoagulant treatment in surgical emergencies[19].
Figure 2. Management of DOACs in relation to surgery timing (modified from[19]). *Andexanet alfa must be administered as a bolus of 30 mg/min in 15 min (low dose) or 30 min (high dose), followed by i.v. infusion of 4 mg (low dose) or 8 mg (high dose) per min for 120 min. DOACs: direct oral anticoagulants.
When the last dose was taken within 2 h prior to arrival in the emergency room, the administration of activated charcoal by oral route has been shown to be effective in reducing absorption by 99.9% for dabigatran, while there is no evidence for factor Xa inhibitors[20].
PCCs represent a heterogeneous combination of coagulation factors and inhibitory components. PCCs typically contain three (II, IX, and X) or four (II, VII, IX, and X) coagulation factors. The overall concentrations of coagulation factor in these preparations are 25 times higher than plasma concentrations. Three- or four-factor concentrates of the PCC demonstrated a discordant effect based on the type of DOAC used: in healthy volunteers, 50 U/kg of four-factor PCC was shown to be effective in reducing PT elongation due to rivaroxaban, while they did not have the same effect for dabigatran-supported aPTT prolongation[21].
The activated prothrombin complex concentrate (aPCC-FEIBA), containing factors II, VII, IX, and X, seems to correct the anticoagulant effect of high doses of rivaroxaban: at high doses (75-80 U/kg), aPCC corrects and promotes the generation of thrombin in vitro on the plasma of healthy volunteers who have taken a single dose of rivaroxaban or dabigatran, and in the blood of healthy volunteers after administration of apixaban[22]. Administration of activated factor VII has not been effective in counteracting bleeding complications in DOAC patients and should be considered as adjuvant therapy during severe bleeding refractory to other treatments.
To date, the only DOAC antagonist drug approved in Europe is idarucizumab, a dabigatran-specific inactivator. It is a humanized monoclonal antibody fragment, which binds to dabigatran with an affinity about 300 times more powerful than dabigatran’s binding affinity with thrombin. As a result of its predominantly renal excretion, the clearance of idarucizumab is reduced in patients with impaired renal function[23]. In total, 202 patients requiring urgent procedure/surgery (Group B) were included in the RE-VERSE AD study. The median age was 78 years, and creatinine clearance averaged 52.6 mL/min[24]. Most patients achieved complete inactivation of dabigatran anticoagulant effect, measured by dilute thrombin time and ecarin clotting time, in the first 4 h after administration of 5 g of idarucizumab. Restoration of hemostasis was achieved in 80.3% of evaluable patients with severe bleeding, while, in patients for whom an emergency procedure was required, normalization of hemostasis was observed in 93.4%[23].
Andexanet, an enzymatically inactive truncated form of factor Xa, has recently been approved by the US Food and Drug Administration (but not yet in Europe) and is capable of binding to direct inhibitors of factor Xa, preventing their anticoagulant action. Although it is still being studied, PER977 (ciraparantag), a small synthetic molecule, seems to be able to bind all new oral anticoagulants. In the study “Andexanet Alfa, a Novel Antidote to the Anticoagulation Effects of FXA Inhibitors 4” (ANNEXA-4), andexanet alfa was successfully used in major or life-threatening bleeding[25]; unlike RE-VERSE-AD, the study did not include patients undergoing emergency surgery.
CONCLUSION
Restoring coagulative activity is mandatory before surgery. In elective-planned surgery, discontinuation of anticoagulation according to guidelines allows for limiting hemorrhagic complications with a low rate of thromboembolic events. No bridge therapy is needed for DOACs, and DVT LMWH prophylactic dose is appropriate for most patients in antivitamin K therapy. Identification of patients at very high risk suitable for bridge therapy is essential in preoperative evaluation. In emergency surgery, rapid reversal of anticoagulation may be obtained by administering specific antidotes or prothrombin complex concentrates, although few studies have been published yet. Finally, for time-dependent surgery, vitamin K allows obtaining INR < 1.5 in most patients within 12 h after administration. Determination of plasma concentration of DOACs after 40-48 h after the last intake may be helpful, particularly in patients who have high bleeding risk surgery or when neuraxial anesthesia is considered.
DECLARATIONS
Authors’ contributionsThe author contributed solely to the article.
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestThe author declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Spyropoulos AC, Bauersachs RM, Omran H, Cohen M. Periprocedural bridging therapy in patients receiving chronic oral anticoagulation therapy. Curr Med Res Opin 2006;22:1109-22.
2. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation 2019;140:e125-51.
3. Ickx BE, Steib A. Perioperative management of patients receiving vitamin K antagonists. Can J Anaesth 2006;53:S113-22.
4. Uotila L. The metabolic functions and mechanism of action of vitamin K. Scand J Clin Lab Invest 1990;201:109-17.
5. Miller CS, Grandi SM, Shimony A, Filion KB, Eisenberg MJ. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol 2012;110:453-60.
6. Gong IY, Kim RB. Importance of pharmacokinetic profile and variability as determinants of dose and response to dabigatran, rivaroxaban, and apixaban. Can J Cardiol 2013;29:S24-33.
7. Spyropoulos AC, Turpie AG, Dunn AS, et al. REGIMEN Investigators. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost 2006;4:1246-52.
8. Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest 2012;141:e326S-50S.
9. Douketis JD. Perioperative management of patients who are receiving warfarin therapy: an evidence-based and practical approach. Blood 2011;117:5044-9.
10. Woods K, Douketis JD, Kathirgamanathan K, Yi Q, Crowther MA. Low-dose oral vitamin K to normalize the international normalized ratio prior to surgery in patients who require temporary interruption of warfarin. J Thromb Thrombolysis 2007;24:93-7.
11. Rechenmacher SJ, Fang JC. Bridging anticoagulation: primum non nocere. J Am Coll Cardiol 2015;66:1392-403.
12. Moores TS, Beaven A, Cattell AE, Baker C, Roberts PJ. Preoperative warfarin reversal for early hip fracture surgery. J Orthop Surg (Hong Kong) 2015;23:33-6.
13. Dentali F, Marchesi C, Giorgi Pierfranceschi M, et al. Safety of prothrombin complex concentrates for rapid anticoagulation reversal of vitamin K antagonists. A meta-analysis. Thromb Haemost 2011;106:429-38.
14. Burbury KL, Milner A, Snooks B, Jupe D, Westerman DA. Short-term warfarin reversal for elective surgery-using low-dose intravenous vitamin K: safe, reliable and convenient*. Br J Haematol 2011;154:626-34.
15. Bhatia M, Talawadekar G, Parihar S, Smith A. An audit of the role of vitamin K in the reversal of International Normalised Ratio (INR) in patients undergoing surgery for hip fracture. Ann R Coll Surg Engl 2010;92:473-6.
16. Heidbuchel H, Verhamme P, Alings M, et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 2015;17:1467-507.
17. Lai A, Davidson N, Galloway SW, Thachil J. Perioperative management of patients on new oral anticoagulants. Br J Surg 2014;101:742-9.
18. Viktil KK, Lehre I, Ranhoff AH, Molden E. Serum concentrations and elimination rates of direct-acting oral anticoagulants (DOACs) in older hip fracture patients hospitalized for surgery: a pilot study. Drugs Aging 2019;36:65-71.
19. Steffel J, Collins R, Antz M, et al. External reviewers. 2021 European heart rhythm association practical guide on the use of non-Vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace 2021;23:1612-76.
20. van Ryn J, Stangier J, Haertter S, et al. Dabigatran etexilate-a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. Thromb Haemost 2010;103:1116-27.
21. Eikelboom JW, Quinlan DJ, van Ryn J, Weitz JI. Idarucizumab: the antidote for reversal of dabigatran. Circulation 2015;132:2412-22.
22. Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation 2011;124:1573-9.
23. Marlu R, Hodaj E, Paris A, Albaladejo P, Cracowski JL, Pernod G. Effect of non-specific reversal agents on anticoagulant activity of dabigatran and rivaroxaban: a randomised crossover ex vivo study in healthy volunteers. Thromb Haemost 2012;108:217-24.
24. Pollack CV Jr, Reilly PA, Eikelboom J, et al. Idarucizumab for dabigatran reversal. N Engl J Med 2015;373:511-20.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Rostagno C. Management of anticoagulant treatment in patients who need non-cardiac surgery. Vessel Plus 2022;6:60. http://dx.doi.org/10.20517/2574-1209.2022.09
AMA Style
Rostagno C. Management of anticoagulant treatment in patients who need non-cardiac surgery. Vessel Plus. 2022; 6: 60. http://dx.doi.org/10.20517/2574-1209.2022.09
Chicago/Turabian Style
Rostagno, Carlo. 2022. "Management of anticoagulant treatment in patients who need non-cardiac surgery" Vessel Plus. 6: 60. http://dx.doi.org/10.20517/2574-1209.2022.09
ACS Style
Rostagno, C. Management of anticoagulant treatment in patients who need non-cardiac surgery. Vessel Plus. 2022, 6, 60. http://dx.doi.org/10.20517/2574-1209.2022.09
About This Article
Copyright
Data & Comments
Data

 Cite This Article 6 clicks
Cite This Article 6 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.