Department of veterans affairs post-coronary artery bypass graft patients' atrial fibrillation: 10-year outcomes
Abstract
Aim: This Department of Veterans Affairs’ (VA) research project evaluated the impact of postoperative atrial fibrillation (POAF) upon 10-year outcomes for coronary artery bypass grafting (CABG) patients.
Methods: Veterans enrolled in the “Randomized On-/Off-pump Bypass” (ROOBY) trial with new-onset POAF post-CABG were compared to those without POAF with respect to 10-year atrial fibrillation (AF) and mortality rates. Multivariable logistic regression examined whether AF was independently associated with 10-year survival after holding other preoperative risk factors constant.
Results: Of the 2203 ROOBY veterans enrolled at 18 VA medical centers from 2002 to 2008, 100 patients with preoperative AF (n = 93) or unknown post-CABG POAF status (n = 7) were excluded. The POAF rate was 26.2%
Conclusion: Post-CABG, ROOBY POAF veterans had higher rates of 10-year AF, which was negatively associated with 10-year survival; however, this association was not significant. Given that POAF may adversely impact 10-year AF rates, additional investigation appears warranted to improve future POAF patients’ care.
Keywords
INTRODUCTION
Patients recovering from coronary artery bypass grafting (CABG) surgery who develop new-onset postoperative atrial fibrillation (POAF) often require an extended hospital stay and increased resource utilization[1-3]. The association of POAF with worse immediate and intermediate-term outcomes is known. As was previously shown, the Randomized On-/Off-Bypass (ROOBY) trial’s patients who developed new-onset POAF had worse short-term outcomes than those without POAF. Complications associated with POAF included reintubation and prolonged ventilation, renal failure, the need for mechanical hemodynamic support, and, ultimately, worse one-year survival and higher costs[1]. For ROOBY patients, POAF was also associated with higher 1-year post-CABG costs, although 5-year costs were comparable[3].
While it is anticipated that most patients who develop POAF after CABG with no underlying history of arrhythmia will revert back to sinus rhythm over time, the actual long-term atrial fibrillation (AF) rates of this post-CABG POAF patient population are not well known. Additionally, the factors associated with long-term AF and long-term survival rates in the POAF population have not been extensively examined. As a ROOBY-FS sub-study, this follow-up investigation builds on prior ROOBY trial reports by examining POAF versus non-POAF patients’ 10-year AF and survival rates with the purpose of determining if POAF impacts these longer-term rates.
METHODS
Briefly summarizing details of the ROOBY trial[4], 2203 veterans were enrolled at 18 VA medical centers between February 2002 and May 2008. These patients were randomized to undergo off-pump vs. on-pump CABG. Evaluated at one year and five years, the clinical endpoints included death, myocardial infarction, and repeat revascularization[5]. For the ROOBY Follow-up Study (ROOBY-FS), the clinical endpoints of death or repeat revascularization were also assessed at 10-years.
As a ROOBY trial approved sub-analysis, patients were examined for the development of new-onset POAF. At one year and five years post-CABG follow-up, clinical outcomes were compared between patients who developed POAF vs. those who did not[1-3].
For these sub-analyses, POAF was defined as any new-onset irregular atrial rhythm lasting longer than 30 minutes, which was similar to the Society of Thoracic Surgeons’ definition of atrial fibrillation. Patients with shorter episodes of atrial fibrillation were excluded, given that the clinical significance of isolated, self-terminating episodes is less certain. Patients with a history of preoperative atrial fibrillation were excluded. This current investigation examined the 10-year rates of AF and death for these two comparative groups. At the time of a 10-year follow-up, ROOBY patients’ AF and vital status were based upon electronic medical records data extracted centrally by the VA Perry Point Cooperative Studies Program (CSP) Coordinating Center’s dedicated nurse coordinators. The VA Corporate Data Warehouse and Medicare databases provided independent verification for chart abstractions performed; additionally, 10-year deaths were verified using both VA and non-VA vital status registries. Discrepancies between databases and chart abstractions were adjudicated by the ROOBY-FS Endpoints Committee (EC); the ROOBY EC included cardiologists, cardiac surgeons, and the CSP nurse coordinator. Using this combined approach to determine survival status, the accuracy rate has been previously reported as > 99%[6].
Statistical analysis
10-year atrial fibrillation status and survival were compared between surviving POAF versus non-POAF patients. Dichotomous variables were compared using either chi-squared analysis or Fisher exact tests. Continuous variables were compared using Student’s t-tests and Wilcoxon rank-sum tests. Kaplan Meier survival were curves compared between POAF vs. non-POAF groups using log-rank tests to evaluate statistical significance. Multivariable logistic regression analysis was performed to identify the patient risk factors associated with 10-year mortality; model eligible variables were screened using P ≤ 0.10. In the regression to predict 10-year death, the final regression model included age, smoking history, chronic obstructive pulmonary disease (COPD), peripheral vascular disease (PVD), hypertension, and renal dysfunction, which was defined as creatinine > 1.5 mg/dL. As this was a ROOBY sub-analysis, the threshold for statistical significance was pre-established at P ≤ 0.01; however, all P-values and 95% confidence intervals have been reported for independent interpretation.
Approval for this ROOBY-FS investigation was obtained through the Perry Point Cooperative Studies Program Coordinating Center (CSPCC), Northport VA Medical Center IRB (Northport, NY), and the Colorado Multiple IRB for the Rocky Mountain Regional VA Medical Center (Aurora, CO). ROOBY IRB Protocol No 1657208 (continuing renewal approved 11/2/2021); ROOBY-FS IRB Protocol No. 1657220 (continuing renewal approved 12/14/2021).
RESULTS
Of the 2203 enrolled patients in ROOBY, 100 were excluded from this sub-analysis due to documented preoperative atrial fibrillation (n = 93) or unknown atrial fibrillation status (n = 7).
Of the 2103 ROOBY patients remaining, 551 patients (26.2%) developed post-CABG new-onset POAF.
Baseline patient characteristics for POAF vs. non-POAF are listed in Table 1. In general, patients who developed POAF were older and had more medical co-morbidities than non-POAF patients.
Patient characteristics at the time of study enrollment
| Baseline patient characteristics | POAF n = 551 | No POAF n = 1552 | P-value |
| Age in years (SD) | 65.3 (8.5) | 62.1 (8.2) | < 0.01 |
| Smoking status | 154 (28%) | 561 (36%) | < 0.01 |
| Chronic obstructive pulmonary disease | 130 (24%) | 297 (19%) | 0.03 |
| Serum Cr ≥ 1.5 | 59 (11%) | 106 (6.8%) | < 0.01 |
| Stroke | 47 (8.5%) | 111 (7.1%) | 0.29 |
| Peripheral vascular disease | 105 (19%) | 218 (14%) | < 0.01 |
| Hypertension | 494 (90%) | 1318 (85%) | < 0.01 |
| Medically treated diabetes | 218 (40%) | 583 (38%) | 0.41 |
| Depression | 62 (11%) | 196 (13%) | 0.46 |
| Ejection fraction ≤ 45% | 80 (15%) | 263 (17%) | 0.18 |
| Urgent surgery | 76 (14%) | 251 (16%) | 0.18 |
| Aortic integrity Good Moderate Poor Unknown | 402 (73%) 107 (19%) 34 (6.2%) 8 (1.4%) | 1225 (79%) 255 (16%) 57 (3.7%) 15 (1.0%) | 0.01 |
| Number of grafts (SD) | 3.0 (0.90) | 2.95 0.93) | 0.02 |
At a 10-year follow-up, 69 patients lacked sufficient detail in the electronic medical record to determine their long-term atrial fibrillation status; these patients were excluded from the current analysis. Among 10-year survivors, atrial fibrillation rates were higher for the POAF group (18.9%, n = 64/338) as compared to the non-POAF group (5.8%, n = 61/1048); P < 0.001.
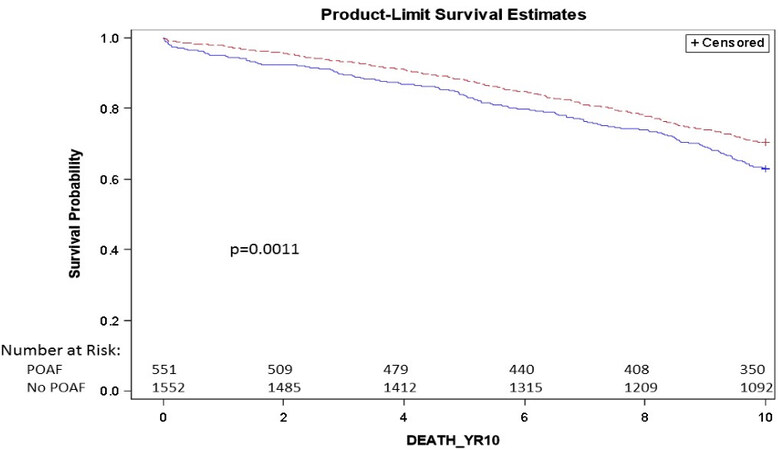
The unadjusted 10-year Kaplan-Meier survival rate for POAF patients was 63%, which was lower than the 70% 10-year survival rate of non-POAF patients [Figure 1]. Factors examined for their association with 10-year survival included age (OR 1.07; 95%CI: 1.06-1.09), COPD (OR 0.65; 95%CI: 0.51-0.82), a preoperative serum creatinine > 1.5 (OR 0.33; 95%CI: 0.23-0.47), PVD (OR 0.45; 95%CI: 0.34-0.58) and smoking (OR 0.57; 95%CI: 0.46-0.72). No association was seen with hypertension (OR 0.89; 95%CI: 0.66-1.20) or POAF (OR 0.95; 95%CI: 0.76-1.19).
DISCUSSION
This investigation found that, of the 26% of patient enrollees in the ROOBY trial who developed POAF after CABG, approximately 19% had AF at 10 years; as such, these patients may benefit from counsel that there is about a 1 in 5 chance of needing long-term anticoagulation and rate control. Patients who did not have POAF had a significantly lower 10-year AF rate of 5.8%. Although the 10-year survival rate of 63% among the POAF patients was also significantly lower than the 70% rate for non-POAF patients, this was unlikely to have been directly related to POAF because it was not found to be independently associated with 10-year risk-adjusted survival using multivariable regression analysis.
These findings appear consistent with the literature examining both the short and long-term incidence of AF and survival among patients with POAF. The incidence of POAF after CABG, approximately 20%-30%, does not appear to have changed significantly over time[7-10]. Patients who developed POAF seem to have higher subsequent rates of AF, as was seen in the current investigation.
While the association of POAF with long-term AF appears consistent, the association with long-term survival is less certain. Much of the literature seems to support an association of POAF with reduced long-term survival. A retrospective study by Thorén and colleagues[8] of 7145 CABG patients (1996 to 2012) followed over a median follow-up of 9.8 years, found an AF rate for the POAF group of 16.2% vs. 5.7 % for non-POAF patients and an association of POAF with overall mortality (HR 1.16; 95%CI: 1.06-1.27), cardiac-specific mortality (HR 1.27; 95%CI: 1.10-1.47), and cerebrovascular mortality (HR 1.39; 95%CI: 1.04-1.86). Similarly, meta-analyses show an association between POAF and mortality. Included is an investigation by Eikelboom and colleagues[10] showing a 10-year mortality rate of 29% among POAF patients (n = 9,389) vs. 23% among non-POAF patients (OR 1.5, 95%CI: 1.4-1.6). Another large-scale meta-analysis[11] of 61 studies (including 188,191 CABG patients) showed mortality rates of 18.6% vs. 13.3% comparing POAF patients vs. no POAF patients, respectively.
However, in other studies, an association of POAF with late AF and reduced long-term survival was not seen. Taha and colleagues’ Swedish registry study of CABG patients (2007 to 2015, n = 24,523) showed no association of POAF with all-cause mortality; adjusted mortality rates were similar to those of non-POAF patients at a median follow up of 4.5 years (adjusted hazard ratio 1.08; 0.98-1.18)[12]. Similarly, our investigation, which examined whether there was an independent association between POAF and survival, did not find one. Rather, the association may have been confounded by other patient factors, such as diabetes, HTN, and COPD, which are more prevalent among patients who develop POAF[13]. In such cases, preoperative identification of these patients and heightened attention to their postoperative management might avert POAF in these cases. Strategies to do so include may include the use of beta-blockers, correcting electrolyte imbalances, and judicious use of inotropes[14]. As well, for patients who do not possess traditionally known risk factors of POAF, research examining serologic markers may provide a useful means of preoperatively identifying patients[15] who are at higher risk for POAF and therefore may benefit from closer attention during their postoperative recovery.
Limitations of this ROOBY 10-year follow-up investigation include the inherent challenges related to its study’s retrospective, observational design. As the 10-year cause of death was not assessed, there was no ability to differentiate noncardiac deaths from cardiac-related causes. Also, death could not be used as a competing event for the comparison of POAF versus non-POAF evaluations of 10-year atrial fibrillation rates. As many risk factors for survival were more prevalent in POAF patients, the 10-year survival comparison between POAF versus non-POAF patients may have been biased. We did not have sufficient granularity to determine the effect of diabetes or hypertension control. As well, the survival curves presented are not risk-adjusted. Unfortunately, data on the use of anti-thrombotic agents, which may impact survival during the 10-year follow-up period, were not collected. Finally, the ROOBY trial’s population consisted primarily of male veterans with multiple co-morbidities; thus, these study results may not be generalizable to women or non-Veteran populations. As regards the former, however, it is noted that POAF may not associate with differences in gender-based survival[16].
These limitations notwithstanding, this ROOBY-FS 10-year investigation shows that patients who experience postoperative atrial fibrillation after CABG are more likely to have 10-year atrial fibrillation and reduced survival at the time of long-term follow-up. At the time of discharge, patients with POAF may benefit from counsel to alert them that it is possible their AF may persist or recur and that assessment and counsel on the risk-benefit ratio of long-term anticoagulation may ultimately be necessary. Patients with POAF who have higher rates of co-morbidities may benefit from prospective studies to determine whether more frequent monitoring and sustained management of these associated health issues could reduce their long-term risk of atrial fibrillation and death.
DECLARATIONS
AcknowledgmentsSpecial thanks to Annette Wiseman, Darlene Kemp and Shirley Lu at the Perry Point Cooperative Studies Program Coordinating Center for their extraordinary administrative, clinical and analytic support as well as to the Research and Development Offices of the Northport VA Medical Center.
Author’s contributionsProvide substantive intellectual manuscript contributions: Quin JA, Almassi GH, Collins JF, Carr BM, Grover FL, Shroyer AL
Conceptualize the design, participate in data acquisition, and help to guide the analytical reports produced, as well as interprete findings: Shroyer AL, Quin JA, Almassi GH
Interprete analytical reports as part of collaborative team discussions: Carr BM, Grover FL
Produce all statistical analytical reports as well as their official interpretation: Collins JF
Drafted the first manuscript and coordinated all manuscript revisions including the final manuscript’s review/approval with all other co-authors (i.e., Shroyer AL, Carr BM, Grover, FL, and Almassi GH): Quin J
Provide review and approval of this final study manuscript: Quin JA, Almassi GH, Collins JF, Carr BM, Grover FL, Shroyer AL
Availability of data and materialsThe ROOBY-FS protocol, published by the New England Journal of Medicine, can be accessed at: https://www.nejm.org/doi/suppl/10.1056/NEJMoa1614341/suppl_file/nejmoa1614341_protocol.pdf. Source documents are available upon written request from Ms. Annette Wiseman at the Department of Veterans Affairs Cooperative Studies Program Coordinating Center in Perry Point, Maryland
Funding for the current study was provided by the Department of Veterans Affairs Cooperative Studies Program through the Cooperative Studies Program Coordinating Center at Perry Point, Maryland (Director Dr. Kousick Biswas and Project Administrator Ms. Annette Wiseman).
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateThis study was conducted in accordance with the Helsinki Declaration with ethical approvals for the ROOBY-FS investigation obtained through the Perry Point Cooperative Studies Program Coordinating Center (CSPCC), Northport VA Medical Center IRB (Northport, NY), and the Colorado Multiple IRB for the Rocky Mountain Regional VA Medical Center (Aurora, CO).
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Almassi GH, Pecsi SA, Collins JF, Shroyer AL, Zenati MA, Grover FL. Predictors and impact of postoperative atrial fibrillation on patients’ outcomes: a report from the Randomized On Versus Off Bypass trial. J Thorac Cardiovasc Surg 2012;143:93-102.
2. Almassi GH, Wagner TH, Carr B, et al. VA #517 Randomized On/Off Bypass (ROOBY) Study Group. Postoperative atrial fibrillation impacts on costs and 1-year clinical outcomes: the Veterans Affairs Randomized On/Off Bypass Trial. Ann Thorac Surg 2015;99:109-14.
3. Almassi GH, Hawkins RB, Bishawi M, et al. Veterans Affairs Randomized On/Off Bypass Follow-up Study (ROOBY-FS) Group. New-onset postoperative atrial fibrillation impact on 5-year clinical outcomes and costs. J Thorac Cardiovasc Surg 2021;161:1803-1810.e3.
4. Shroyer AL, Grover FL, Hattler B, et al. Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37.
5. Shroyer, AL, Hattler B, Wagner TH, et al. 5-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med 2017;377(7):623-32.
6. Quin JA, Hattler B, Shroyer ALW, et al. Department of Veteran Affairs (CSP#517-FS) ROOBY Follow-up Study’s Endpoints Committee. Concordance between administrative data and clinical review for mortality in the randomized on/off bypass follow-up study (ROOBY-FS). J Card Surg 2017;32:751-6.
7. Filardo G, Pollock BD, da Graca B, et al. Lower survival after coronary artery bypass in patients who had atrial fibrillation missed by widely used definitions. Mayo Clin Proc Innov Qual Outcomes 2020;4:630-7.
8. Thorén E, Wernroth ML, Christersson C, Grinnemo KH, Jidéus L, Ståhle E. Compared with matched controls, patients with postoperative atrial fibrillation (POAF) have increased long-term AF after CABG, and POAF is further associated with increased ischemic stroke, heart failure and mortality even after adjustment for AF. Clin Res Cardiol 2020;109:1232-42.
9. Michniewicz E, Mlodawska E, Lopatowska P, Tomaszuk-Kazberuk A, Malyszko J. Patients with atrial fibrillation and coronary artery disease - double trouble. Adv Med Sci 2018;63:30-5.
10. Eikelboom R, Sanjanwala R, Le ML, Yamashita MH, Arora RC. Postoperative atrial fibrillation after cardiac surgery: a systematic review and meta-analysis. Ann Thorac Surg 2021;111:544-54.
11. Woldendorp K, Farag J, Khadra S, Black D, Robinson B, Bannon P. Postoperative atrial fibrillation after cardiac surgery: a meta-analysis. Ann Thorac Surg 2021;112:2084-93.
12. Taha A, Nielsen SJ, Bergfeldt L, et al. New-onset atrial fibrillation after coronary artery bypass grafting and long-term outcome: a population-based nationwide study from the SWEDEHEART registry. J Am Heart Assoc 2021;10:e017966.
13. Seo EJ, Hong J, Lee HJ, Son YJ. Perioperative risk factors for new-onset postoperative atrial fibrillation after coronary artery bypass grafting: a systematic review. BMC Cardiovasc Disord 2021;21:418.
14. Omar A, Ehab M Elshihy, Mahmoud Singer, David Zarif, Omar Dawoud. Perioperative risk factors predisposing to atrial fibrillation after cabg surgery. Heart Surg Forum 2021;24:E402-6.
15. Li XY, Hou HT, Chen HX, et al. Preoperative plasma biomarkers associated with atrial fibrillation after coronary artery bypass surgery. J Thorac Cardiovasc Surg 2021;162:851-863.e3.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Quin JA, Almassi GH, Collins JF, Carr BM, Grover FL, Shroyer ALW. Department of veterans affairs post-coronary artery bypass graft patients' atrial fibrillation: 10-year outcomes. Vessel Plus 2022;6:41. http://dx.doi.org/10.20517/2574-1209.2021.119
AMA Style
Quin JA, Almassi GH, Collins JF, Carr BM, Grover FL, Shroyer ALW. Department of veterans affairs post-coronary artery bypass graft patients' atrial fibrillation: 10-year outcomes. Vessel Plus. 2022; 6: 41. http://dx.doi.org/10.20517/2574-1209.2021.119
Chicago/Turabian Style
Quin, Jacquelyn A., G. Hossein Almassi, Joseph F. Collins, Brendan M. Carr, Frederick L. Grover, A. Laurie W. Shroyer. 2022. "Department of veterans affairs post-coronary artery bypass graft patients' atrial fibrillation: 10-year outcomes" Vessel Plus. 6: 41. http://dx.doi.org/10.20517/2574-1209.2021.119
ACS Style
Quin, JA.; Almassi GH.; Collins JF.; Carr BM.; Grover FL.; Shroyer ALW. Department of veterans affairs post-coronary artery bypass graft patients' atrial fibrillation: 10-year outcomes. Vessel Plus. 2022, 6, 41. http://dx.doi.org/10.20517/2574-1209.2021.119
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 8 clicks
Cite This Article 8 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.