Calm the raging hormone - a new therapeutic strategy involving progesterone-signaling for hemorrhagic CCMs
Abstract
Cerebral cavernous malformations (CCMs), one of the most common vascular malformations, are characterized by abnormally dilated intracranial microvascular capillaries resulting in increased susceptibility to hemorrhagic stroke. As an autosomal dominant disorder with incomplete penetrance, the majority of CCMs gene mutation carriers are largely asymptomatic, but, when symptoms occur, the disease has typically reached the stage of focal hemorrhage with irreversible brain damage, while the molecular “trigger” initiating the occurrence of CCM pathology remain elusive. Currently, the invasive neurosurgery removal of CCM lesions is the only option for the treatment, despite the recurrence of worse symptoms frequently occurring after surgery. Therefore, there is a grave need for the identification of molecular targets for therapeutic treatment and biomarkers as risk predictors for hemorrhagic stroke prevention. Based on the various perturbed angiogenic signaling cascades mediated by the CCM signaling complex (CSC) reported, there have been many proposed candidate drugs, targeting potentially angiogenic-relevant signaling pathways dysregulated by loss of function of one of the CCM proteins, which might not be enough to correct the pathological phenotype, hemorrhagic CCMs. In this review, we describe a new paradigm for the mechanism of hemorrhagic CCM lesions and propose a new concept for the assurance of CSC stability to prevent the devastating outcome of hemorrhagic CCMs.
Keywords
INTRODUCTION
Cerebral cavernous malformations (CCMs) are characterized by abnormally dilated intracranial microvascular capillaries that result in increased susceptibility to stroke[1-5]. Familial CCMs are an autosomal dominant condition[1,6]. Three genes have been identified as culprits of most familial CCM cases[7-16]: CCM1 at 7q11-22[11], CCM2 at 7p15-23[12], and CCM3 at 3q25.2-27[12]. These genes encode CCM proteins, including KRIT1 as CCM1[13,16-19], MGC4607 as CCM2[20], and PDCD10 as CCM3[21,22], that have been shown to interact with each other and form a core CCM triplex. In this triplex, CCM1 and CCM3 compete to bind to PTB domains of CCM2[23]. This core CCM triplex, in turn, interacts with other proteins[22,24-27] to form a complex referred to as the CCM signaling complex (CSC)[28,29]. Although the majority of CCMs gene mutation carriers are largely asymptomatic due to the incomplete penetrance of CCMs, when symptoms do occur, the disease has typically reached a serious stage of focal hemorrhage with irreversible brain damage. Currently, the invasive neurosurgical removal of CCM lesions is the only option for treatment, despite the recurrence of hemorrhagic events after surgery. Therefore, there is a grave need to understand the angiogenic functions of CSC in maintaining neurovascular integrity. Uncovering the mechanistic underpinnings of this signalosome may provide novel avenues for developing stroke prevention and vascular therapy techniques. Based on the various perturbed angiogenic signaling cascades reported, there have been many proposed candidate drugs, potentially targeting angiogenic-relevant signaling pathways dysregulated by loss of function of one of the CCM proteins, which might not be enough to correct the pathological phenotype, hemorrhagic CCMs. In this article, we propose a new concept for the assurance of CSC stability to prevent the devastating outcome of hemorrhagic CCMs.
FEMALE SEX STEROID HORMONES AND STROKE
The overall lifetime risk of stroke is similar between women and men[30]; however, postmenopausal women are at a much greater stroke risk, compared to premenopausal women. Women generally bear a notable lower risk of stroke during earlier life, until reaching their middle age, doubling the risk of stroke in women 10 years post-menopause[31-33]. This drastically increased stroke risk in women is caused by declining levels of circulating sex steroid hormones in the blood, especially estrogen[31,34]. Estrogen has been widely recognized as a beneficial factor for the integrity of vasculature[35-42] due to its actions on nuclear/membrane estrogen receptors (nERs/mERs)[37,43-45] in vascular smooth muscle cells[46,47] and endothelial cells[38,48-50]. Furthermore, sex steroids, estrogen, androgen, and glucocorticoid, have been evaluated, but no significant perturbation of CSC was found involving any of these sterols[51]. Increased stroke risk associated with altered levels of circulating female sex hormones has been well defined for several major female physiological events, including post-menopause, pregnancy, oral contraceptive regimens, and hormone replacement therapy[52]. It needs to be mentioned that the physiological changes during pregnancy, caused by the altered levels/composition of circulating female sex hormones, is a major risk factor for stroke in women[53-60]. Epidemiologic data in the United States indicate that approximately 87% of strokes are ischemic, and the remaining 13% are hemorrhagic strokes[61-63]. Interestingly, hemorrhagic stroke is the most dominant type (up to 74%) of strokes during pregnancy, much higher than that in the general population[64-71], suggesting an important correlation between altered progesterone (PRG) levels [Table 1] and elevated hemorrhagic stroke risk[72].
Expected normal-range PRG values from serum/plasma samples in various age groups of both women and men
| Physiological stages (women) | Values for ELISA kit detection |
| Follicular phase | 0.2-1.4 ng/mL |
| Luteal phase | 4.0-25 ng/mL |
| Menopause | 0.1-1.0 ng/mL |
| Normal men | 0.1-1.0 ng/mL |
Although women and men have measurable amounts of PRG in the bloodstream, the levels and patterns of change of circulating PRG differ. Circulating PRG is approximately 0.5 ng/mL for males, while PRG levels vastly fluctuate between 4.0 and 25 ng/mL for premenopausal women during the luteal phase of their menstrual cycle [Table 1][72]. Only 2% of total blood PRG is in its free, active form, which has a very short half-life (5-10 min)[73]. Over 98% of PRG in the blood is believed to be physiologically inactive and passively transported by blood proteins[74], mainly by two major PRG-binding proteins: serpin A6 (binds ~18% of PRG) and albumin (binds ~80% of PRG)[75-77].
CSC COUPLES BOTH CLASSIC AND NON-CLASSIC PRG RECEPTOR SIGNALING
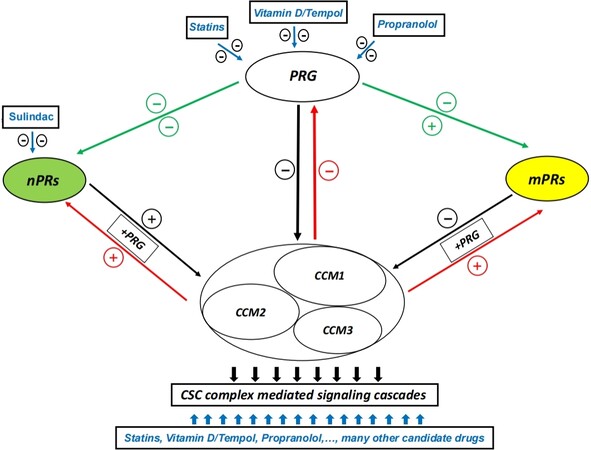
As a sex steroid hormone, PRG elicits its cellular responses through two major signaling pathways. PRG binds to either nuclear progesterone receptors (nPRs) to enact classic PRG effects[78] or to membrane progesterone receptors (mPRs/PAQRs)[79,80] and PRG receptor membrane components[81,82] to enact non-classic PRG effects. Currently, the intricate balance and switch mechanisms between these two signaling cascades remain unknown. Recently, we found that CSC can modulate PRG receptor-mediated signaling, coupling both classic and non-classic signaling by establishing crosstalk between them in nPR positive (+) breast cancer T47D cells. Based on our findings, under PRG actions, CSC stability is regulated by two major signaling cascades: (1) by the negative effects of PRG or its antagonist (nPRs only), mifepristone, via both classes of PRG receptors; and (2) by the positive effects of nPRs signaling[51]. This discovery reveals that the balance between classic and non-classic PRG signaling impacts CSC function and identifies CSC as an important mediator of nPR and mPR crosstalk in nPR(+) cells. Our observation is further supported by a previous finding that PRG can act simultaneously on both nPRs and mPRs, and the activation of mPR signaling can potentiate the hormone-activated nPR-2 isoform[78]. The intricate feedback regulation among the PRG-activated CSC-mPRs-PRG-nPRs (CmPn) signaling network in nPR(+) T47D cells can be summarized as a common mechanism that exists among the CmPn signaling network under steroid actions[51]. In this CmPn signaling network, PRG and its nPR-specific antagonist, MIF, work independently or synergistically to disrupt CSC through their common targets, mPRs, in a backward fashion (CSC←mPRs←PRG) [Figure 1][51].
Figure 1. Schematic representation of the relationship among the CmPn network and potential candidate drug targets. The relationship among CSC, PRG, and two types of PRG receptors (nPRs and mPRs) is illustrated based on our current data. Candidate drug targeting points are presented with blue arrows, where candidate drugs are highlighted with blue letters within the box. Green arrow-lines indicate effects of PRG on PRG receptors, black arrow-lines indicate effects of PRG and its receptors on CSC, and red arrow-lines indicate effects of the CSC on biogenesis of PRG and its receptors. +PRG indicates under steroid actions. The + symbol indicates observed enhancement, while the - symbol demonstrates an inhibitory effect. CCM: Cerebral cavernous malformation; CSC: CCM signaling complex; PRG: progesterone; nPRs: nuclear progesterone receptors; mPRs: membrane receptors.
A COMMON REGULATORY MECHANISM UNDERLYING THE PROMOTIVE EFFECTS OF CSC ON MPRS IN BREAST CANCER CELLS
PRG can activate downstream signaling in both nPR(+) and nPR(-) cells by binding to mPRs[51,83-85]. Distinct from nPRs, mPRs represent a unique class of membrane steroid receptors that mediate non-classic PRG actions in nPR(+) and nPR(-) cells[78,86]. Numerous studies have implicated mPRs in breast cancer[87-95], especially nPR(-) breast cancers[84,88,93]. After defining the CmPn signaling network in nPR(+) breast cancer T47D cells[51], we shifted our focus to two nPR(-) breast cancer cells (MDA-MB231 and MDA-MB468), both of which are triple-negative breast cancer (TNBC) cells. Using these two nPR(-) cell models, we confirmed the presence of the CSC-mPRs-PRG (CmP) signaling network in nPR(-) breast cancer cells[96]. We also demonstrated that a common core mechanism exists among nPR(-) breast cancer cells, termed the CmP signaling network. In the CmP signaling network, CSC can stabilize mPRs under steroid actions in a forward fashion (CSC→mPRs), which overlaps with the CmPn signaling network in nPR(+) breast cancer cells under steroid actions, regardless of nPR(+/-) cell type. This implicates a more essential role of CSC on the stability of mPRs in nPR(-) cells under steroid actions[96]. Our data support the previous findings that multiple mPRs can be co-expressed in various mammalian cell types[78,83,93,97,98] to perform multifaceted non-classic PRG signaling cascades among different nPR(+/-) mammalian cells[93].
ANGIOGENIC RESPONSES TO SEX STEROID ACTIONS THROUGH MPRS SIGNALING IN NPR(-) VASCULAR ENDOTHELIAL CELLS
CCMs are more common in women and become symptomatic during their reproductive period (in their 30s and 40s)[99,100]. Although no conclusive results have been found[101], hormonal changes during pregnancy have long been suspected as significant factors for increased bleeding[102-104], and female gender is a key risk factor for bleeding in CCM patients[102,105]. Increases in the size of CCM lesions[106-109] and the elevated frequency of hemorrhagic CCMs during pregnancy have been well documented[103,110-115], suggesting that pregnancy is associated with an increased risk of hemorrhagic CCMs. It has long been speculated that the flux of hormones during pregnancy may predispose CCMs to hemorrhage[102,111-114], and, furthermore, increased PRG levels during early pregnancy[116,117] have been indicated to enhance the progression of lesions[118], possibly through the induction of structural changes within vessels[119]. Increased risk for acute CCM bleedings[101,103,104,113,115,120] or formation of a de novo CCM lesion[113,120,121] have also been reported during pregnancy. Collectively, these findings reinforce the idea that there is gender- and sex hormone-associated differences in hemorrhagic stroke pathophysiology and suggest that PRG-mediated signaling should be further investigated. Interestingly, nPR(+) endothelial cells (ECs) can only be found in the veins and lymphatics of the uterus and ovaries, where human umbilical vein endothelial cells (HUVECs) are derived[122]. Additionally, the MEKK3-KLF-ADAMTS signaling pathway has been implicated in CSC-mediated angiogenic activities[123]. KLFs are largely expressed in reproductive tissues and have been implicated as co-regulators and integrators of progesterone/progesterone receptor transactivity[124]. There are some associations between progesterone and ADAMTS-1 demonstrating ADAMTS as a transcriptional target of progesterone actions mainly in the ovaries of nPR-KO mice[125]. Additionally, in Xenopus laevis eggs and embryos, it was demonstrated that progesterone can stimulate JNK activation through both MEK/p42 MAPK-dependent and -independent pathways, and the addition of progesterone induced synthesis of MAPKKK c-Mos, leading to the activation of the MEK1-ERK-RSK cascade[126]. However, there is currently no available literature systemically demonstrating the effects of progesterone on the MEKK3-KLF-ADAMTS signaling pathway. The vast majority of vascular ECs derived from other tissues are nPR(-) and mPRs(+), where only non-classic actions of PRG have been reported[82]. When we used combined steroids (PRG + MIF) to treat four nPRs(-) microvascular ECs and nPRs(+) HUVECs, again, our data support a common regulatory mechanism underlying the inhibitory effects of PRG/MIF on CSC, independent of nPRs. In addition, the sex hormone inhibition of CCM1/3 protein expression in ECs is more dramatic than in non-endothelial-derived cell lines[51,127], reaffirming that steroid hormones have much stronger actions on the stability of CSC through mPRs in ECs.
PRG ACTIONS INCREASED PERMEABILITY OF EC MONOLAYER AND COMPROMISED BBB INTEGRITY
The haploinsufficiency of CCM proteins in microvascular ECs is an essential step in the pathogenesis of CCM lesions, as demonstrated by in vivo studies with zebrafish[128,129] and Ccms mice models[130-132], but it is insufficient to form hemorrhagic CCMs. Although the “two-hit” model, which creates a null condition in the lesion, can be used to explain familial CCM cases, it fails to account for sporadic forms of CCM, which make up 80% of all CCM cases[133]. Additional studies have demonstrated that haploinsufficiency condition of CCMs are insufficient in initiating hemorrhagic events of CCM lesions[134]. Since the “two-hit” model alone cannot explain CCM ruptures, there must be a molecular “trigger” that initiates the hemorrhagic events of CCM lesions. Therefore, we performed both in vivo and in vitro permeability assays demonstrating significantly increased blood-brain barrier (BBB) permeability among all Ccms (1, 2, 3) mutants only in the hormone treatment groups, compared to WT and/or untreated Ccms (1, 2, 3) mutants mice, which was further supported by in vitro permeability assays showing increased permeability of different EC lines under steroid actions, compared to vehicle controls[51,127]. This concordant BBB leakage among all Ccms mutant mice was not seen in other treatment groups, nor that of other tested organs, indicating that chronic steroid actions specifically increase BBB permeability, and it is the primary mechanism underlying CCM lesion formation. Therefore, we concluded that BBB integrity among individuals with CCMs deficiency is particularly susceptible to chronic and elevated sex steroid actions[51].
PARADIGM SHIFT FOR HEMORRHAGIC EVENTS IN CCMS OPENS UP NEW AVENUES OF RESEARCH
Hemorrhage is often rooted in defective endothelial cell junctions, and microvessel rupture is a result of compromised BBB integrity[135]. Currently, two major theories for the induction of hemorrhagic CCMs are the anticoagulant vascular domain theory and the gut microbiota theory. In the anticoagulant vascular domain theory, local increases in the endothelial cofactors that generate anticoagulant activated protein C contribute to recurrent bleeding in CCM lesions[136]. In the gut microbiota theory, Gram-negative bacterial signaling through the lipopolysaccharide-activated innate immune receptor, Toll-like receptor 4, promotes hemorrhagic bleeding in both Ccm1/2 mutant mice, indicating the important roles for the gut microbiome and innate immune signaling in the pathogenesis of CCMs[134]. The gut microbiota theory focuses on the importance of gut microbiota in influencing the interaction direction by inducing an inflammatory gut milieu, which leads to systemic inflammation that exacerbates the inflammatory response in the brain and promotes detrimental effects on the BBB[137]. However, lipopolysaccharide-induced Ccms hemorrhagic mice demonstrate massive bleeding, leading to lethality at the early stages of life, uncharacteristic of human CCMs. Nonetheless, neither of the previous theories addresses a key issue of gender discrepancies in CCM pathogenesis, demanding further evaluation for the underlying mechanisms of hemorrhagic stroke. Although it is still under debate[4,112,138], female dominance in CCM patients has long been suggested[3,113,139,140], and consensus has been reached on more severe bleeding with worse neurological outcomes in females[102,139]. This aggressive course of hemorrhagic lesions in females has been proposed to be a consequence of endocrine influences[3,113,139,140]. Our data demonstrate that enhanced PRG-mPRs signaling, due to perturbed homeostasis of PRG, leads to BBB disruption, in addition to evidence that long exposure to hormonal contraceptives increases the risk of cerebral venous sinus thrombosis[141], which is incongruent with the anticoagulant vascular domain theory[136]. Our findings that immunosuppression, caused by sex steroid actions in Ccms deficient mice, is associated with CCM bleeding also disagree with the gut microbiota theory[134]. Therefore, we propose a new paradigm for the mechanisms of initiating hemorrhagic CCMs. In nPR(-) ECs, the feedback loops among CSC-mPRs-PRG actions appear to be sensitive, and perturbation of this intricate balance [Figure 1][127], such as hormone therapy or hormonal contraception regimens, could result in an increased risk for BBB disruption, especially for human CCMs mutant carriers. Our new paradigm provides a theory that is in line with clinically observed CCM conditions and demonstrates the important functions of CSC and non-classic PRG actions in angiogenesis and vascular health.
CURRENT PHARMACOLOGICAL CANDIDATES TARGETING HEMORRHAGIC CCMS LINKED TO PRG HOMEOSTASIS
Since the molecular and cellular mechanism of the CmP network in microvascular ECs remains largely unknown, we recently investigated the CmP signaling network in nPR(-) ECs[127]. Our data indicate that nPR(-) ECs are different from nPR(-) TNBC cells (TNBC cells have extremely low CCM expression). Although nPR(-) ECs share a common core mechanism between the newly defined CmP network and the CmPn network in breast cancer cells, nPR(-) ECs also showed that steroids can disrupt CSC through their common targets, mPRs, in a backward fashion (CSC←mPRs←PRG), identical to nPR(+) breast cancer cells[51], indicating the significant impact of steroid actions on the stability of CSC.
Many candidate drugs have been identified and tested in animal models and even small clinical trials[142,143]. Ironically, the current pool of very diverse candidate drugs were collectively gathered as certain specific blockers for signaling pathways identified from different experiments using various in vitro and/or in vivo models[144-157]. Among them, statins and propranolol advanced into clinical trials[142,143,158], due to some promising data. Propranolol, one of the most commonly used β-adrenoceptor blockers (beta-blockers), was first used to successfully treat another common vascular condition, infantile hemangioma in 2008[159], and additionally with major success in three later cases of giant infantile cerebral cavernomas[160-162]. Utilizing in vitro, histological, and clinical findings, it was demonstrated that 20-60 mg/day of propranolol not only was effective in reducing previous hemorrhagic lesions, but it also prevented new hemorrhage in familial CCM patients and reduced lesion size and edema in occipital CCM patients[144]. Additionally, it was also observed that propranolol therapy was effective in immediately stabilizing progressing lesions and preventing future bleeds in sporadic CCM patients[163]. Currently, there are two clinical trials actively recruiting patients to assess lesion burden and clinical events in both familial and symptomatic cerebral cavernous malformation patients[142]. Statin use has been shown to reduce both nonfatal and fatal strokes, improve functional outcomes after ischemic strokes, and reduce coronary death rate and primary and secondary cardiovascular events[164-167]. A randomized controlled trial involving the use of high-dose statin therapy demonstrated a 16% decrease in total stroke as well as a five-year absolute risk reduction in fatal and nonfatal strokes[167]. Despite the promising results seen with statin therapy, a post hoc analysis demonstrated a significant increase in intracerebral hemorrhage, suggesting that high-dose statin therapy may have contradictory results[167,168]. These results demonstrate a potential therapeutic use of statins for stroke prevention, but it should be tailored on an individual patient basis to ensure benefits are maximized while risks are minimized.
Intriguingly, by examining these candidate drugs, we found an interesting association of these candidates with the circulating levels of PRG, especially the ones with promising data in animal models. While tempol can alleviate increased PRG levels induced by dehydroepiandrosterone (DHEA, not statistically significant)[169], vitamin D, as a close physiological partner with PRG[170], is a strong inhibitor of PRG production[171], suggesting the inhibitory effect of vitamin D/tempol on PRG production. As an inhibitor for TGFβ/β-catenin signaling, sulindac inhibits the expression level of classic PRG receptors (nPRs)[172], while other TGFβ signaling inhibitors, such as K02288 (TGFβ/BMP6)[173], DMH1 (BMP6)[174], and SB431542 (BMP6)[173], have no effect on PRG levels, suggesting that TGFβ inhibitors might not be a good choice for PRG inhibition. Intriguingly, the two most promising candidates, which have been put in clinical trials, show strong inhibitory effects on PRG levels. While PRG can abolish the beneficial effects of atorvastatin on vascular EC functions[175], statins (atorvastatin, simvastatin, lovastatin, and mevastatin) can directly inhibit PRG levels[176,177]. Although the molecular mechanisms of its therapeutic action are still unknown, its known effect of vasoconstriction may be involved[178,179]. Propranolol has been reported to have an inhibitory effect on PRG levels, from both direct[180,181] and indirect[182,183] evidence, indicating the possibility of decreased PRG levels in this therapeutic process. Finally, although these two candidate drugs (statins and propranolol) show great potential for PRG inhibition[176,177,180-183], they might not be suitable drugs for the treatment and/or prevention of hemorrhagic CCMs. As common drugs for vascular conditions, both are highly effective and safe for most people, but they have been shown to have some side effects due to their wide spectrum of targets. Extensive clinical trials are needed to determine their real benefit and efficacy for hemorrhagic CCMs.
CONCLUSION
As mentioned above, the haploinsufficiency of CCM genes in microvascular ECs is an essential step in the pathogenesis of CCM lesions, as demonstrated by in vivo studies with zebrafish[128,129] and Ccms mice models[130-132], but it is insufficient to form hemorrhagic CCMs, mimicking the incomplete penetrance seen in human CCMs. However, when symptoms occur, the disease has typically reached the stage of focal hemorrhage (likely close to CCM-null condition at the genomic level and/or loss of function at the proteomic level) with irreversible brain damage. Following this rationale, we believe it could be strategic to suppress PRG actions on capillary ECs in order to prevent haploinsufficiency of CCM genes reaching similar levels observed in CCM loss-of-function for the initiation of a hemorrhagic event. Furthermore, it is not surprising to observe the widespread perturbation of almost all known signaling cascades involved in angiogenesis due to deficiency of CCMs, since CSC is an essential regulator of microvascular angiogenesis and perturbation of CSC will lead to disrupted angiogenesis in the most fundamental way[29,128,129,184,185]. For this reason, efforts to try to correct any specific dysregulated angiogenic signaling, rooted from deficiency in any CCMs, to alleviate CCM lesion burden or even prevent hemorrhagic CCMs might eventually prove to be too little too late [Figure 1].
DECLARATIONS
Authors’ contributionsConceptualization, methodology, writing original draft preparation, reviewing and editing: Zhang J
Writing, reviewing and editing: Abou-Fadel JS
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestBoth authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2021.
REFERENCES
1. Rigamonti D, Drayer BP, Johnson PC, Hadley MN, Zabramski J, Spetzler RF. The MRI appearance of cavernous malformations (angiomas). J Neurosurg 1987;67:518-24.
2. Otten P, Pizzolato GP, Rilliet B, Berney J. 131 cases of cavernous angioma (cavernomas) of the CNS, discovered by retrospective analysis of 24,535 autopsies. Neurochirurgie 1989;2:82-3,128.
3. Moriarity JL, Clatterbuck RE, Rigamonti D. The natural history of cavernous malformations. Neurosurg Clin N Am 1999;10:411-7.
4. Curling O Jr, Kelly DL Jr, Elster AD, Craven TE. An analysis of the natural history of cavernous angiomas. J Neurosurg 1991;75:702-8.
5. Batra S, Lin D, Recinos PF, Zhang J, Rigamonti D. Cavernous malformations: natural history, diagnosis and treatment. Nat Rev Neurol 2009;5:659-70.
6. Rigamonti D, Spetzler RF, Drayer BP, et al. Appearance of venous malformations on magnetic resonance imaging. J Neurosurg 1988;69:535-9.
7. Dubovsky J, Zabramski JM, Kurth J, et al. A gene responsible for cavernous malformations of the brain maps to chromosome 7q. Hum Mol Genet 1995;4:453-8.
8. Marchuk DA, Gallione CJ, Morrison LA, et al. A locus for cerebral cavernous malformations maps to chromosome 7q in two families. Genomics 1995;28:311-4.
9. Günel M, Awad IA, Finberg K, et al. Genetic heterogeneity of inherited cerebral cavernous malformation. Neurosurgery 1996;38:1265-71.
10. Günel M, Awad IA, Anson J, Lifton RP. Mapping a gene causing cerebral cavernous malformation to 7q11.2-q21. Proc Natl Acad Sci U S A 1995;92:6620-4.
11. Johnson EW, Iyer LM, Rich SS, et al. Refined localization of the cerebral cavernous malformation gene (CCM1) to a 4-cM interval of chromosome 7q contained in a well-defined YAC contig. Genome Res 1995;5:368-80.
12. Craig HD, Günel M, Cepeda O, et al. Multilocus linkage identifies two new loci for a mendelian form of stroke, cerebral cavernous malformation, at 7p15-13 and 3q25.2-27. Hum Mol Genet 1998;7:1851-8.
13. Laberge-le Couteulx S, Jung HH, Labauge P, et al. Truncating mutations in CCM1, encoding KRIT1, cause hereditary cavernous angiomas. Nat Genet 1999;23:189-93.
14. Laberge S, Labauge P, Maréchal E, Maciazek J, Tournier-Lasserve E. Genetic heterogeneity and absence of founder effect in a series of 36 French cerebral cavernous angiomas families. Eur J Hum Genet 1999;7:499-504.
15. Dupré N, Verlaan DJ, Hand CK, et al. Linkage to the CCM2 locus and genetic heterogeneity in familial cerebral cavernous malformation. Can J Neurol Sci 2003;30:122-8.
16. Zhang J, Clatterbuck RE, Rigamonti D, Dietz HC. Mutations in KRIT1 in familial cerebral cavernous malformations. Neurosurgery 2000;46:1272-7; discussion 1277.
17. Sahoo T, Johnson EW, Thomas JW, et al. Mutations in the gene encoding KRIT1, a Krev-1/rap1a binding protein, cause cerebral cavernous malformations (CCM1). Hum Mol Genet 1999;8:2325-33.
18. Eerola I, Plate KH, Spiegel R, Boon LM, Mulliken JB, Vikkula M. KRIT1 is mutated in hyperkeratotic cutaneous capillary-venous malformation associated with cerebral capillary malformation. Hum Mol Genet 2000;9:1351-5.
19. Verlaan DJ, Siegel AM, Rouleau GA. Krit1 missense mutations lead to splicing errors in cerebral cavernous malformation. Am J Hum Genet 2002;70:1564-7.
20. Liquori CL, Berg MJ, Siegel AM, et al. Mutations in a gene encoding a novel protein containing a phosphotyrosine-binding domain cause type 2 cerebral cavernous malformations. Am J Hum Genet 2003;73:1459-64.
21. Bergametti F, Denier C, Labauge P, et al. Mutations within the programmed cell death 10 gene cause cerebral cavernous malformations. Am J Hum Genet 2005;76:42-51.
22. Ma X, Zhao H, Shan J, et al. PDCD10 interacts with Ste20-related kinase MST4 to promote cell growth and transformation via modulation of the ERK pathway. Mol Biol Cell 2007;18:1965-78.
23. Jiang X, Padarti A, Qu Y, et al. Alternatively spliced isoforms reveal a novel type of PTB domain in CCM2 protein. Sci Rep 2019;9:15808.
24. Uhlik MT, Abell AN, Johnson NL, et al. Rac-MEKK3-MKK3 scaffolding for p38 MAPK activation during hyperosmotic shock. Nat Cell Biol 2003;5:1104-10.
25. Hilder TL, Malone MH, Bencharit S, et al. Proteomic identification of the cerebral cavernous malformation signaling complex. J Proteome Res 2007;6:4343-55.
26. Voss K, Stahl S, Schleider E, et al. CCM3 interacts with CCM2 indicating common pathogenesis for cerebral cavernous malformations. Neurogenetics 2007;8:249-56.
27. Zawistowski JS, Stalheim L, Uhlik MT, et al. CCM1 and CCM2 protein interactions in cell signaling: implications for cerebral cavernous malformations pathogenesis. Hum Mol Genet 2005;14:2521-31.
28. Zhang J, Rigamonti D, Dietz HC, Clatterbuck RE. Interaction between krit1 and malcavernin: implications for the pathogenesis of cerebral cavernous malformations. Neurosurgery 2007;60:353-9; discussion 359.
29. Padarti A, Zhang J. Recent advances in cerebral cavernous malformation research. Vessel Plus 2018;2:21.
30. Sealy-Jefferson S, Wing JJ, Sánchez BN, et al. Age- and ethnic-specific sex differences in stroke risk. Gend Med 2012;9:121-8.
31. Lisabeth L, Bushnell C. Stroke risk in women: the role of menopause and hormone therapy. Lancet Neurol 2012;11:82-91.
32. Lisabeth L, Bushnell C. Stroke risk in women: the role of menopause and hormone therapy. Lancet Neurol 2012;11:125.
33. Lisabeth LD, Baek J, Morgenstern LB, et al. Sex differences in the impact of acute stroke treatment in a population-based study: a sex-specific propensity score approach. Ann Epidemiol 2017;27:493-8.e2.
34. Shekhar S, Travis OK, He X, Roman RJ, Fan F. Menopause and ischemic stroke: a brief review. MOJ Toxicol 2017;3:00059.
35. Blum A, Cannon RO 3rd. Effects of oestrogens and selective oestrogen receptor modulators on serum lipoproteins and vascular function. Curr Opin Lipidol 1998;9:575-86.
36. Komesaroff PA, Fullerton M, Esler MD, Dart A, Jennings G, Sudhir K. Low-dose estrogen supplementation improves vascular function in hypogonadal men. Hypertension 2001;38:1011-6.
37. Ness KF, Sharif I, Macpherson S et al. Modification of vascular function by the oestrogen receptor beta: the effect of ageing. Brit J Pharmacol 2002; doi: 10.1046/j.1365-201x.2002.00992.x.
39. Djordjevic N, Babic G, Ognjanovic B, et al. Estrogen improves vascular function in preeclampsia via ROS reduction. Febs Journal 2012;279:429-112.
40. O'Donnell E, Goodman JM, Morris BL, Floras JS, Harvey PJ. Abnormal vascular function in physically active estrogen deficient premenopausal women is not rectified by acute dynamic exercise. Circulation 2012;126:A15561.
41. Tiyerili V, Mueller CM, Nickenig G, Becher UM. Estrogen improves vascular function and morphology via peroxisome-proliferator-activated-receptor gamma. Eur Heart J 2012;33:279.
42. Tiyerili V, Müller CF, Fung S, Panek D, Nickenig G, Becher UM. Estrogen improves vascular function via peroxisome-proliferator-activated-receptor-γ. J Mol Cell Cardiol 2012;53:268-76.
43. Meyer MR, Haas E, Prossnitz ER, Barton M. Non-genomic regulation of vascular cell function and growth by estrogen. Mol Cell Endocrinol 2009;308:9-16.
44. Su EJ, Lin ZH, Zeine R, et al. Estrogen receptor-beta mediates cyclooxygenase-2 expression and vascular prostanoid levels in human placental villous endothelial cells. Am J Obstet Gynecol 2009;200:427.e1-427.e4278.
45. Zhu Y, Bian Z, Lu P, et al. Abnormal vascular function and hypertension in mice deficient in estrogen receptor beta. Science 2002;295:505-8.
46. Cignarella A, Minici C, Brusadelli A, Bolego C, Maggi A, Puglisi L. 4P-1045 Estrogen receptor expression in vascular smooth muscle cells is altered by diabetes: implications for inducible NO synthase function. Atherosclerosis Supplements 2003;4:304.
47. Lee CH, Su SC, Chiang CF, et al. Estrogen modulates vascular smooth muscle cell function through downregulation of SIRT1. Oncotarget 2017;8:110039-51.
48. White CR, Shelton J, Chen SJ, et al. Estrogen restores endothelial cell function in an experimental model of vascular injury. Circulation 1997;96:1624-30.
49. Gavin KM, Seals DR, Silver AE, Moreau KL. Vascular endothelial estrogen receptor alpha is modulated by estrogen status and related to endothelial function and endothelial nitric oxide synthase in healthy women. J Clin Endocrinol Metab 2009;94:3513-20.
50. Moreau KL, Stauffer BL, Kohrt WM, Seals DR. Essential role of estrogen for improvements in vascular endothelial function with endurance exercise in postmenopausal women. J Clin Endocrinol Metab 2013;98:4507-15.
51. Abou-Fadel J, Jiang X, Grajeda B, et al. CCM signaling complex (CSC) coupling both classic and non-classic progesterone receptor signaling. bioRxiv 2020; doi: 10.1101/2020.05.24.112847.
52. Rantanen K, Tatlisumak T. Stroke in women - oral contraception, pregnancy, and hormone replacement therapy. Curr Vasc Pharmacol 2013:11 58-73.
53. Beal CC, Faucher MA. Stroke and pregnancy: an integrative review with implications for neuroscience nurses. J Neurosci Nurs 2015;47:76-84; quiz E1.
54. Carbillon L. Pregnancy is an essential spontaneous screening stress test for the risk of early stroke in women. Stroke 2008;39:e138.
55. Caso V, Falorni A, Bushnell CD, et al. Pregnancy, hormonal treatments for infertility, contraception, and menopause in women after ischemic stroke: a consensus document. Stroke 2017;48:501-6.
56. Cheng CA, Lee JT, Lin HC, et al. Pregnancy increases stroke risk up to 1 year postpartum and reduces long-term risk. QJM 2017;110:355-60.
58. James AH, Bushnell CD, Jamison MG, Myers ER. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol 2005;106:509-16.
59. Jeng JS, Tang SC, Yip PK. Incidence and etiologies of stroke during pregnancy and puerperium as evidenced in Taiwanese women. Cerebrovasc Dis 2004;18:290-5.
60. Sanders BD, Davis MG, Holley SL, Phillippi JC. Pregnancy-associated stroke. J Midwifery Womens Health 2018;63:23-32.
61. Rosamond W, Flegal K, Furie K, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008;117:e25-146.
62. Rosamond W, Flegal K, Furie K, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2010;122:e10.
63. Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997;349:1269-76.
64. Ban L, Abdul Sultan A, Stephansson O, et al. The incidence of first stroke in and around pregnancy: a population-based cohort study from Sweden. Eur Stroke J 2017;2:250-6.
66. Leffert LR, Clancy CR, Bateman BT, et al. Patient characteristics and outcomes after hemorrhagic stroke in pregnancy. Circ Cardiovasc Qual Outcomes 2015;8:S170-8.
68. Liu XJ, Wang S, Zhao YL, Zhang D, Zhao JZ. A single-center study of hemorrhagic stroke caused by cerebrovascular disease during pregnancy and puerperium in China. Int J Gynaecol Obstet 2011;113:82-3.
69. Miller EC, Sundheim KM, Willey JZ, Boehme AK, Agalliu D, Marshall RS. The impact of pregnancy on hemorrhagic stroke in young women. Cerebrovasc Dis 2018;46:10-5.
70. Ulrich ND, Lapeyre ER, Moore RC. Hemorrhagic stroke resulting from venous malformation at 20 weeks of pregnancy. Ochsner J 2016;16:542-4.
71. Yoshida K, Takahashi JC, Takenobu Y, Suzuki N, Ogawa A, Miyamoto S. Strokes associated with pregnancy and puerperium: a nationwide study by the Japan stroke society. Stroke 2017;48:276-82.
72. Filicori M, Butler JP, Crowley WF Jr. Neuroendocrine regulation of the corpus luteum in the human. Evidence for pulsatile progesterone secretion. J Clin Invest 1984;73:1638-47.
73. Aufrère MB, Benson H. Progesterone: an overview and recent advances. J Pharm Sci 1976;65:783-800.
74. Hammond GL. Potential functions of plasma steroid-binding proteins. Trends Endocrinol Metab 1995;6:298-304.
75. Cox RM, McGlothlin JW, Bonier F. Evolutionary endocrinology: hormones as mediators of evolutionary phenomena: an introduction to the symposium. Integr Comp Biol 2016;56:121-5.
76. Diczfalusy E, Crosignani PG. Introduction: from reproductive endocrinology to reproductive health. The short history of a new departure by ESHRE. European Society for Human Reproduction and Embryology. Hum Reprod 1996;11:1776-7.
77. Yasumizu K, Kato J. Introduction to obstetrical endocrinology. 23. Sex differentiation and hormones. Josanpu Zasshi 1985;39:168-73. (in Japanese).
78. Karteris E, Zervou S, Pang Y, et al. Progesterone signaling in human myometrium through two novel membrane G protein-coupled receptors: potential role in functional progesterone withdrawal at term. Mol Endocrinol 2006;20:1519-34.
79. Tokumoto T, Tokumoto M, Oshima T, et al. Characterization of multiple membrane progestin receptor (mPR) subtypes from the goldfish ovary and their roles in the induction of oocyte maturation. Gen Comp Endocrinol 2012;177:168-76.
80. Tokumoto T, Hossain MB, Wang J. Establishment of procedures for studying mPR-interacting agents and physiological roles of mPR. Steroids 2016;111:79-83.
81. Jiang C, Zuo F, Wang Y, et al. Progesterone exerts neuroprotective effects and improves long-term neurologic outcome after intracerebral hemorrhage in middle-aged mice. Neurobiol Aging 2016;42:13-24.
82. Simoncini T, Mannella P, Fornari L, et al. Differential signal transduction of progesterone and medroxyprogesterone acetate in human endothelial cells. Endocrinology 2004;145:5745-56.
83. Dosiou C, Hamilton AE, Pang Y, et al. Expression of membrane progesterone receptors on human T lymphocytes and Jurkat cells and activation of G-proteins by progesterone. J Endocrinol 2008;196:67-77.
84. Pang Y, Thomas P. Progesterone signals through membrane progesterone receptors (mPRs) in MDA-MB-468 and mPR-transfected MDA-MB-231 breast cancer cells which lack full-length and N-terminally truncated isoforms of the nuclear progesterone receptor. Steroids 2011;76:921-8.
85. Sleiter N, Pang Y, Park C, et al. Progesterone receptor A (PRA) and PRB-independent effects of progesterone on gonadotropin-releasing hormone release. Endocrinology 2009;150:3833-44.
86. Zuo L, Li W, You S. Progesterone reverses the mesenchymal phenotypes of basal phenotype breast cancer cells via a membrane progesterone receptor mediated pathway. Breast Cancer Res 2010;12:R34.
87. Dressing GE, Lange CA. Integrated actions of progesterone receptor and cell cycle machinery regulate breast cancer cell proliferation. Steroids 2009;74:573-6.
88. Dressing GE, Thomas P. Identification of membrane progestin receptors in human breast cancer cell lines and biopsies and their potential involvement in breast cancer. Steroids 2007;72:111-6.
89. Adam PJ, Boyd R, Tyson KL, et al. Comprehensive proteomic analysis of breast cancer cell membranes reveals unique proteins with potential roles in clinical cancer. J Biol Chem 2003;278:6482-9.
90. Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 2012;490:61-70.
91. Castelnovo LF, Magnaghi V, Thomas P. Expression of membrane progesterone receptors (mPRs) in rat peripheral glial cell membranes and their potential role in the modulation of cell migration and protein expression. Steroids 2019;142:6-13.
92. Charles NJ, Thomas P, Lange CA. Expression of membrane progesterone receptors (mPR/PAQR) in ovarian cancer cells: implications for progesterone-induced signaling events. Horm Cancer 2010;1:167-76.
93. Dressing GE, Alyea R, Pang Y, Thomas P. Membrane progesterone receptors (mPRs) mediate progestin induced antimorbidity in breast cancer cells and are expressed in human breast tumors. Horm Cancer 2012;3:101-12.
94. Jiang G, Zhang S, Yazdanparast A, et al. Comprehensive comparison of molecular portraits between cell lines and tumors in breast cancer. BMC Genomics 2016;17 Suppl 7:525.
95. Zhao Y, Ruan X, Wang H, et al. The presence of a membrane-bound progesterone receptor induces growth of breast cancer with norethisterone but not with progesterone: a xenograft model. Maturitas 2017;102:26-33.
96. Abou-Fadel J, Grajeda B, Jiang X, et al. CmP signaling network unveils novel biomarkers for triple negative breast cancer in African American women. bioRxiv 2021; doi: 10.1101/2021.05.24.445510.
97. Thomas P, Pang Y. Membrane progesterone receptors: evidence for neuroprotective, neurosteroid signaling and neuroendocrine functions in neuronal cells. Neuroendocrinology 2012;96:162-71.
98. Nutu M, Weijdegård B, Thomas P, Thurin-Kjellberg A, Billig H, Larsson DG. Distribution and hormonal regulation of membrane progesterone receptors beta and gamma in ciliated epithelial cells of mouse and human fallopian tubes. Reprod Biol Endocrinol 2009;7:89.
99. Canavero S. Intramedullary cavernous angiomas of the spinal cord: clinical presentation, pathological features, and surgical management. Neurosurgery 1993;32:692-3.
100. Ogilvy CS, Louis DN, Ojemann RG. Intramedullary cavernous angiomas of the spinal cord: clinical presentation, pathological features, and surgical management. Neurosurgery 1992;31:219-29; discussion 229.
101. Burkhardt JK, Bozinov O, Nürnberg J, et al. Neurosurgical considerations on highly eloquent brainstem cavernomas during pregnancy. Clin Neurol Neurosurg 2012;114:1172-6.
102. Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T. Natural history of intracranial cavernous malformations. J Neurosurg 1995;83:56-9.
103. Awada A, Watson T, Obeid T. Cavernous angioma presenting as pregnancy-related seizures. Epilepsia 1997;38:844-6.
104. Porter RW, Detwiler PW, Spetzler RF, et al. Cavernous malformations of the brainstem: experience with 100 patients. J Neurosurg 1999;90:50-8.
105. Gross BA, Lin N, Du R, Day AL. The natural history of intracranial cavernous malformations. Neurosurg Focus 2011;30:E24.
106. Kalani MY, Zabramski JM. Risk for symptomatic hemorrhage of cerebral cavernous malformations during pregnancy. J Neurosurg 2013;118:50-5.
107. Witiw CD, Abou-Hamden A, Kulkarni AV, Silvaggio JA, Schneider C, Wallace MC. Cerebral cavernous malformations and pregnancy: hemorrhage risk and influence on obstetrical management. Neurosurgery 2012;71:626-30; discussion 631.
108. Yamasaki T, Handa H, Yamashita J, et al. Intracranial and orbital cavernous angiomas. A review of 30 cases. J Neurosurg 1986;64:197-208.
109. Zauberman H, Feinsod M. Orbital hemangioma growth during pregnancy. Acta Ophthalmol (Copenh) 1970;48:929-33.
110. Flemming KD, Goodman BP, Meyer FB. Successful brainstem cavernous malformation resection after repeated hemorrhages during pregnancy. Surg Neurol 2003;60:545-7.
111. Katayama Y, Tsubokawa T, Maeda T, Yamamoto T. Surgical management of cavernous malformations of the third ventricle. J Neurosurg 1994;80:64-72.
112. Porter PJ, Willinsky RA, Harper W, Wallace MC. Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage. J Neurosurg 1997;87:190-7.
113. Pozzati E, Acciarri N, Tognetti F, Marliani F, Giangaspero F. Growth, subsequent bleeding, and de novo appearance of cerebral cavernous angiomas. Neurosurgery 1996;38:662-70.
114. Robinson JR, Awad IA, Little JR. Natural history of the cavernous angioma. J Neurosurg 1991;75:709-14.
115. Safavi-Abbasi S, Feiz-Erfan I, Spetzler RF, et al. Hemorrhage of cavernous malformations during pregnancy and in the peripartum period: causal or coincidence? Neurosurg Focus 2006;21:e12.
116. Tibbetts TA, Mendoza-Meneses M, O'Malley BW, Conneely OM. Mutual and intercompartmental regulation of estrogen receptor and progesterone receptor expression in the mouse uterus. Biol Reprod 1998;59:1143-52.
117. Tan J, Paria BC, Dey SK, Das SK. Differential uterine expression of estrogen and progesterone receptors correlates with uterine preparation for implantation and decidualization in the mouse. Endocrinology 1999;140:5310-21.
118. Schwartz TH, Hibshoosh H, Riedel CJ. Estrogen and progesterone receptor-negative T11 vertebral hemangioma presenting as a postpartum compression fracture: case report and management. Neurosurgery 2000;46:218-21.
119. Morello A, Tumbiolo A, Pinto G, Lo Duca B. Cavernous angioma of the spinal dura. J Neurosurg Sci 1991;35:31-5.
120. Yamada S, Nakase H, Nakagawa I, Nishimura F, Motoyama Y, Park YS. Cavernous malformations in pregnancy. Neurol Med Chir (Tokyo) 2013;53:555-60.
121. Detwiler PW, Porter RW, Zabramski JM, Spetzler RF. De novo formation of a central nervous system cavernous malformation: implications for predicting risk of hemorrhage. Case report and review of the literature. J Neurosurg 1997;87:629-32.
122. Goddard LM, Murphy TJ, Org T, et al. Progesterone receptor in the vascular endothelium triggers physiological uterine permeability preimplantation. Cell 2014;156:549-62.
123. Zhou Z, Rawnsley DR, Goddard LM, et al. The cerebral cavernous malformation pathway controls cardiac development via regulation of endocardial MEKK3 signaling and KLF expression. Dev Cell 2015;32:168-80.
124. Simmen RC, Heard ME, Simmen AM, et al. The Krüppel-like factors in female reproductive system pathologies. J Mol Endocrinol 2015;54:R89-R101.
125. Robker RL, Russell DL, Espey LL, Lydon JP, O'Malley BW, Richards JS. Progesterone-regulated genes in the ovulation process: ADAMTS-1 and cathepsin L proteases. Proc Natl Acad Sci U S A 2000;97:4689-94.
126. Bagowski CP, Xiong W, Ferrell JE Jr. c-Jun N-terminal kinase activation in Xenopus laevis eggs and embryos. A possible non-genomic role for the JNK signaling pathway. J Biol Chem 2001;276:1459-65.
127. Abou-Fadel J, Jiang X, Padarti A, et al. CCM signaling complex (CSC) is a master regulator governing homeostasis of progesterone and its mediated signaling cascades. bioRxiv 2020; doi: 10.1101/2020.06.10.145003.
128. Liu H, Rigamonti D, Badr A, Zhang J. Ccm1 assures microvascular integrity during angiogenesis. Transl Stroke Res 2010;1:146-53.
129. Liu H, Rigamonti D, Badr A, Zhang J. Ccm1 regulates microvascular morphogenesis during angiogenesis. J Vasc Res 2011;48:130-40.
130. Whitehead KJ, Plummer NW, Adams JA, Marchuk DA, Li DY. Ccm1 is required for arterial morphogenesis: implications for the etiology of human cavernous malformations. Development 2004;131:1437-48.
131. Boulday G, Blécon A, Petit N, et al. Tissue-specific conditional CCM2 knockout mice establish the essential role of endothelial CCM2 in angiogenesis: implications for human cerebral cavernous malformations. Dis Model Mech 2009;2:168-77.
132. Plummer NW, Squire TL, Srinivasan S, et al. Neuronal expression of the Ccm2 gene in a new mouse model of cerebral cavernous malformations. Mamm Genome 2006;17:119-28.
133. Cohen-Gadol AA, Jacob JT, Edwards DA, Krauss WE. Coexistence of intracranial and spinal cavernous malformations: a study of prevalence and natural history. J Neurosurg 2006;104:376-81.
134. Tang AT, Choi JP, Kotzin JJ, et al. Endothelial TLR4 and the microbiome drive cerebral cavernous malformations. Nature 2017;545:305-10.
135. Clatterbuck RE, Eberhart CG, Crain BJ, Rigamonti D. Ultrastructural and immunocytochemical evidence that an incompetent blood-brain barrier is related to the pathophysiology of cavernous malformations. J Neurol Neurosurg Psychiatry 2001;71:188-92.
136. Lopez-Ramirez MA, Pham A, Girard R, et al. Cerebral cavernous malformations form an anticoagulant vascular domain in humans and mice. Blood 2019;133:193-204.
137. Argaw AT, Asp L, Zhang J, et al. Astrocyte-derived VEGF-A drives blood-brain barrier disruption in CNS inflammatory disease. J Clin Invest 2012;122:2454-68.
138. Kondziolka D, Lunsford LD, Kestle JR. The natural history of cerebral cavernous malformations. J Neurosurg 1995;83:820-4.
139. Maraire JN, Awad IA. Intracranial cavernous malformations: lesion behavior and management strategies. Neurosurgery 1995;37:591-605.
140. Moriarity JL, Wetzel M, Clatterbuck RE, et al. The natural history of cavernous malformations: a prospective study of 68 patients. Neurosurgery 1999;44:1166-71; discussion 1172.
141. Amoozegar F, Ronksley PE, Sauve R, Menon BK. Hormonal contraceptives and cerebral venous thrombosis risk: a systematic review and meta-analysis. Front Neurol 2015;6:7.
142. Flemming KD, Lanzino G. Cerebral cavernous malformation: what a practicing clinician should know. Mayo Clin Proc 2020;95:2005-20.
143. Chohan MO, Marchiò S, Morrison LA, et al. Emerging pharmacologic targets in cerebral cavernous malformation and potential strategies to alter the natural history of a difficult disease: a review. JAMA Neurol 2019;76:492-500.
144. Zabramski JM, Kalani MYS, Filippidis AS, Spetzler RF. Propranolol treatment of cavernous malformations with symptomatic hemorrhage. World Neurosurg 2016;88:631-9.
145. Zabramski JM. In reply to the letter to the editor regarding "Propranolol treatment of cavernous malformations with symptomatic hemorrhage". World Neurosurg 2021;145:513.
146. You C, Zhao K, Dammann P, et al. EphB4 forward signalling mediates angiogenesis caused by CCM3/PDCD10-ablation. J Cell Mol Med 2017;21:1848-58.
147. Wüstehube J, Bartol A, Liebler SS, et al. Cerebral cavernous malformation protein CCM1 inhibits sprouting angiogenesis by activating DELTA-NOTCH signaling. Proc Natl Acad Sci U S A 2010;107:12640-5.
148. Olesen SH, Zhu JY, Martin MP, Schönbrunn E. Discovery of diverse small-molecule inhibitors of mammalian sterile20-like kinase 3 (MST3). ChemMedChem 2016;11:1137-44.
149. Marchi S, Corricelli M, Trapani E, et al. Defective autophagy is a key feature of cerebral cavernous malformations. EMBO Mol Med 2015;7:1403-17.
150. Maddaluno L, Rudini N, Cuttano R, et al. EndMT contributes to the onset and progression of cerebral cavernous malformations. Nature 2013;498:492-6.
151. Gibson CC, Zhu W, Davis CT, et al. Strategy for identifying repurposed drugs for the treatment of cerebral cavernous malformation. Circulation 2015;131:289-99.
152. Bravi L, Rudini N, Cuttano R, et al. Sulindac metabolites decrease cerebrovascular malformations in CCM3-knockout mice. Proc Natl Acad Sci U S A 2015;112:8421-6.
153. Aguilera D, Tomita T, Goldman S, Fangusaro J. Incidental resolution of a radiation-induced cavernous hemangioma of the brain following the use of bevacizumab in a child with recurrent medulloblastoma. Pediatr Neurosurg 2010;46:303-7.
154. Weiner GM, Ducruet AF. Fasudil slows development of cavernous malformations. Neurosurgery 2017;80:N25-7.
155. Shenkar R, Shi C, Austin C, et al. RhoA kinase inhibition with fasudil versus simvastatin in murine models of cerebral cavernous malformations. Stroke 2017;48:187-94.
156. McDonald DA, Shi C, Shenkar R, et al. Fasudil decreases lesion burden in a murine model of cerebral cavernous malformation disease. Stroke 2012;43:571-4.
157. De Luca E, Pedone D, Moglianetti M, et al. Multifunctional platinum@BSA-Rapamycin nanocarriers for the combinatorial therapy of cerebral cavernous malformation. ACS Omega 2018;3:15389-98.
158. Zhao L. New concepts regarding the treatment of cerebral cavernous malformations with symptomatic hemorrhage using propranolol. World Neurosurgery 2019;124:466.
159. Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Boralevi F, Thambo JB, Taïeb A. Propranolol for severe hemangiomas of infancy. N Engl J Med 2008;358:2649-51.
160. Berti I, Marchetti F, Skabar A, Zennaro F, Zanon D, Ventura A. Propranolol for cerebral cavernous angiomatosis: a magic bullet. Clin Pediatr (Phila) 2014;53:189-90.
161. Moschovi M, Alexiou GA, Stefanaki K, Tourkantoni N, Prodromou N. Propranolol treatment for a giant infantile brain cavernoma. J Child Neurol 2010;25:653-5.
162. Cavalheiro S, Campos HG, Silva da Costa MD. A case of giant fetal intracranial capillary hemangioma cured with propranolol. J Neurosurg Pediatr 2016;17:711-6.
163. Reinhard M, Schuchardt F, Meckel S, et al. Propranolol stops progressive multiple cerebral cavernoma in an adult patient. J Neurol Sci 2016;367:15-7.
164. Ridker PM, Danielson E, Fonseca FA, et al. JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008;359:2195-207.
165. Hong KS, Lee JS. Statins in acute ischemic stroke: a systematic review. J Stroke 2015;17:282-301.
166. Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebocontrolled trial. Lancet 2002;360:7-22.
167. Amarenco P, Bogousslavsky J, Callahan A 3rd, et al. Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006;355:549-59.
168. Goldstein LB, Amarenco P, Szarek M, et al. SPARCL Investigators. Hemorrhagic stroke in the stroke prevention by aggressive reduction in cholesterol levels study. Neurology 2008;70:2364-70.
169. Li T, Zhang T, Gao H, et al. Tempol ameliorates polycystic ovary syndrome through attenuating intestinal oxidative stress and modulating of gut microbiota composition-serum metabolites interaction. Redox Biol 2021;41:101886.
170. Monastra G, De Grazia S, De Luca L, Vittorio S, Unfer V. Vitamin D: a steroid hormone with progesterone-like activity. Eur Rev Med Pharmacol Sci 2018;22:2502-12.
171. Hong SH, Lee JE, Kim HS, et al. Effect of vitamin D3 on production of progesterone in porcine granulosa cells by regulation of steroidogenic enzymes. J Biomed Res 2016;30:203-8.
172. Lim JT, Joe AK, Suzui M, Shimizu M, Masuda M, Weinstein IB. Sulindac sulfide and exisulind inhibit expression of the estrogen and progesterone receptors in human breast cancer cells. Clin Cancer Res 2006;12:3478-84.
173. Mattar D, Samir M, Laird M, Knight PG. Modulatory effects of TGF-β1 and BMP6 on thecal angiogenesis and steroidogenesis in the bovine ovary. Reproduction 2020;159:397-408.
174. Chang HM, Cheng JC, Klausen C, Leung PC. BMP15 suppresses progesterone production by down-regulating StAR via ALK3 in human granulosa cells. Mol Endocrinol 2013;27:2093-104.
175. Faludi AA, Aldrighi JM, Bertolami MC, et al. Progesterone abolishes estrogen and/or atorvastatin endothelium dependent vasodilatory effects. Atherosclerosis 2004;177:89-96.
176. Kaur K, N Allahbadia G, Singh M. Use of 20mg statins (atorvastatin/simvastatin) as a novel new option of medically treating fibroids-overcoming the drawback of selective progesterone receptor modulators of interruption before long term use. IPCB 2019:5.
177. Rung E, Friberg PA, Shao R, et al. Progesterone-receptor antagonists and statins decrease de novo cholesterol synthesis and increase apoptosis in rat and human periovulatory granulosa cells in vitro. Biol Reprod 2005;72:538-45.
178. Osada A, Araki E, Yamashita Y, Ishii T. Combination therapy of propranolol, levothyroxine, and liothyronine was effective in a case of severe consumptive hypothyroidism associated with infantile hepatic hemangioma. Clin Pediatr Endocrinol 2019;28:9-14.
179. Frongia G, Byeon JO, Mehrabi A, Günther P. Recurrence rate of infantile hemangioma after oral propranolol therapy. Eur J Pediatr 2021;180:585-90.
180. Wheeler AG, Walker M, Lean J. Influence of adrenergic receptors on ovarian progesterone secretion in the pseudopregnant cat and oestradiol secretion in the oestrous cat. J Reprod Fertil 1987;79:195-205.
181. Wheeler AG, Lean J, Walker M. Peripheral progesterone concentrations in the luteal-phase ewe: effects of a beta-adrenergic receptor antagonist and two beta 2-adrenergic agonists. J Endocrinol 1988;116:137-42.
182. Fylling P. Dexamethasone or propranolol blockade of induced increase in plasma progesterone in early human pregnancy. Acta Endocrinol (Copenh) 1973;72:569-72.
183. Fernández-guasti A, Larsson K, Beyer C. Prevention of progesterone-induced lordosis behavior by alpha or beta adrenergic antagonists in ovariectomized estrogen-primed rats. Pharmacol Biochem Behav 1985;22:279-82.
184. Zhang J. . Molecular biology of cerebral cavernous malformation. In: Rigamonti D, editor. Cavernous Malformations of the Nervous System. Cambridge University Press; 2011. p. 31-40.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Zhang J, Abou-Fadel JS. Calm the raging hormone - a new therapeutic strategy involving progesterone-signaling for hemorrhagic CCMs. Vessel Plus 2021;5:48. http://dx.doi.org/10.20517/2574-1209.2021.64
AMA Style
Zhang J, Abou-Fadel JS. Calm the raging hormone - a new therapeutic strategy involving progesterone-signaling for hemorrhagic CCMs. Vessel Plus. 2021; 5: 48. http://dx.doi.org/10.20517/2574-1209.2021.64
Chicago/Turabian Style
Zhang, Jun, Johnathan S. Abou-Fadel. 2021. "Calm the raging hormone - a new therapeutic strategy involving progesterone-signaling for hemorrhagic CCMs" Vessel Plus. 5: 48. http://dx.doi.org/10.20517/2574-1209.2021.64
ACS Style
Zhang, J.; Abou-Fadel JS. Calm the raging hormone - a new therapeutic strategy involving progesterone-signaling for hemorrhagic CCMs. Vessel Plus. 2021, 5, 48. http://dx.doi.org/10.20517/2574-1209.2021.64
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 22 clicks
Cite This Article 22 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.