Contemporary indications for percutaneous revascularization of coronary chronic total occlusions
Abstract
Chronic total occlusions (CTO) are frequently encountered during coronary angiography, and are generally regarded as the most challenging coronary lesions for percutaneous coronary intervention (PCI). Despite great technical advancements and greatly improved reported procedural success rates during previous years, data on clinical benefit of these procedures still remain scarce and controversial. Data from observational trials suggested that PCI for CTO could be linked to improvements both in symptoms and hard cardiovascular outcomes, while randomized controlled trials showed symptomatic improvement only, without improvement in patient’s prognosis. This is in parallel with findings for non-CTO PCI in patients with stable angina. Having in mind complexity of these interventions, high costs, greater volume of contrast, and radiation exposure, appropriate patient selection is crucial for optimizing treatment effectiveness. There are few important factors that should be taken into consideration before planning and attempting PCI for CTO. These are: severity of patient’s symptoms despite optimal medical therapy, presence of inducible myocardial ischemia and/or viability in the territory of occluded coronary artery.
Keywords
Introduction
Chronic total occlusions (CTO) of coronary artery is defined as an occluded coronary vessel with thrombolysis in myocardial infarction flow 0, that lasts for 3 months or more[1,2]. They are often found during coronary angiography, with a prevalence rate of 18%-52%[3-5].
CTO remain the most challenging lesion subset in patients undergoing percutaneous coronary interventions (PCI). It was early recognized as one of the most important obstacle in achieving complete revascularization in patients with multivessel coronary artery disease. Even the father of interventional cardiology Andreas Gruentzig noted in an interview in 1985 (two weeks before his tragic passing in an airplane crash): “The total closure is a real problem, if we cannot solve the total closure problem, we probably will never really address the question of multivessel disease dilatation”[6].
Myocardial territory distal to CTO is usually supplied by collateral flow, which is sometimes sufficient to preserve viability and contractile function in resting conditions. On the contrary, collaterals are most often not sufficient to provide adequate blood flow during increased demands, providing adequate protection against ischemia in only 5% of patients[7]. This means that collateral vessels cannot fully substitute the function of open epicardial artery, which constitutes the rationale for performing PCI for CTO.
Regarding the prognostic impact of coronary artery bypass grafting (CABG) for CTO revascularization, this issue is lacking high-quality randomized data. Isolated CABG for an isolated CTO of the LAD (or other coronary arteries) cannot be justified on the basis of preventing future events compared with either medical therapy or PCI. CABG for CTOs will often be part of a strategy of offering complete revascularization[8].
Technical aspects of the PCI for CTO
Although PCI for CTO remains most challenging for many interventionalists, we are witnessing gradual improvement in all procedural aspects during last decade. For experienced operators, procedural success rates could reach > 90%, which is the result of improvements in instrumentaria, better training, increasing operator expertise with complex techniques, and spreading the knowledge through the work of dedicated CTO organizations, such as EuroCTO club and others[9-12].
Many technical factors should be taken into consideration while planning PCI for CTO[2]. In general, ad hoc PCI for CTO is not encouraged; instead, staged, elective, and carefully planned approach is preferred. When dealing with selection of arterial access site, most dedicated CTO operators prefer to use femoral artery for targeting occluded artery, since it allows them to use larger size catheters (7 or 8 French) which offers better passive support and more space for simultaneous insertion of devices. Radial artery is most often used to cannulate non-CTO artery in order to visualize occluded artery distal to the place of occlusion via collateral circulation. Dual injection should be used whenever possible, since it allows operator to appropriately asses morphologic characteristics of the occluded segment. Selection of coronary guidewires is critical step for the successful PCI of CTO. Many characteristics of the guidewires should be taken into account when selecting appropriate guidewire like: polymer cover, wire coating, core material, and tip stiffness. Operators may choose between wires depending of what they need most in every phase of intervention: more torque control, more maneuverability, more penetration power, less potential to damage collateral channels, reentry etc. Microcatheters are devices that are almost always used in PCI for CTO. They offer the operator possibility to exchange guidewires rapidly, provides additional support for the guidewire, provides protection of collateral vessel, provide route to inject small amount of contrast (“tip injection”) to visualize distal vessel or collaterals. Many improvements in manufacturing technology give us wide array of available devices that meet different needs of operators in various situations. Contralateral contrast injection is frequently needed to precisely and safely navigate guidewire toward vessel distal to occlusion, and we strongly recommend using it whenever distal vessel cannot be adequately visualized via ipsilateral dye injection.
Traditionally, antegrade approach is used as a first strategy of CTO recanalization. With the development of new guidewires, microcatheters, the single wire techniques, parallel-wire technique, techniques with subintimal tracking, and antegrade dissection and reentry technique, it remained the most common first choice strategy. Retrograde techniques were developed over long period of time, and made major breakthrough in mid 2000s with the pioneering work of Dr Osamu Katoh who introduced the Controlled Antegrade and Retrograde subintimal Tracking technique of retrograde CTO recanalization. Detailed consideration of choosing between antegrade and retrograde strategies is beyond the scope of this review, and may be found elsewhere[13]. It is worth mentioning few more aspects specific to PCI for CTO. In a recently published report from OPEN-CTO registry, major complication rates still remain significant and higher than in non-CTO PCI: in-hospital/one-month mortality was 0.9% and 1.3%, respectively, while coronary perforations requiring treatment occurred in 4.8% of patients[14]. Operators should be aware of contrast toxicity and should limit the contrast volume to minimum needed and adjusted to renal function of the patient. Radiation safety is an important issue and physicians should make every effort to reduce radiation exposure, and to document radiation exposure during a PCI procedure.
Symptomatic and prognostic impact of the PCI for CTO
Despite these truly amazing technical improvements in achieving proficiency of CTO recanalization, many aspects of clinical efficacy of this demanding procedure remain controversial. Several non-randomized (observational) trials have shown that successful CTO revascularization could be linked to improved cardiovascular outcomes[15-17] and better quality of life (QOL)[18,19]. We have recently published a long term (66 months) follow-up of cohort of 283 patients in whom recanalization of CTO was attempted[20]. Patients with successfully recanalized CTO had lower rate of MACE (defined as composite of cardiac mortality, myocardial infarction, and target vessel revascularization) than patients with failed procedure; the difference that remained statistically significant after adjustment for baseline between-group differences using propensity scores (adjusted HR 0.402; 95%CI: 0.196-0.824; P = 0.013). Christakopoulos et al.[21] published a review of 25 observational trials and showed improved outcomes with successful PCI of the CTO (which included survival, angina severity, and the need for coronary artery bypass surgery). Having in mind all limitation of these kind of trials, no causal inferences could be drawn between PCI for CTO and positive cardiac outcomes. These conclusions may be regarded only as a hypothesis generating, and must be checked in appropriately designed randomized controlled clinical trials (RCTs). Only RCTs could answer questions related to causality between the procedure and outcomes, and we have data from few of them recently published.
The EXPLORE (Evaluating Xience and Left Ventricular Function in PCI on Occlusions After ST-Elevation Myocardial Infarction) study randomized 304 patients presented as STEMI which also had a CTO lesion in a non-infarct artery to additional PCI of CTO soon after primary PCI or optimal medical therapy only[22]. Primary endpoints were left ventricular ejection fraction (LVEF) and left ventricular end diastolic volume (LVEDV) on cardiac MRI after 4 months. Authors did not report any benefit for CTO PCI in terms of LVEF (44.1% ± 12.2% vs. 44.8% ± 11.9%; P = 0.60) or LVEDV (215.6 ± 62.5 mL vs. 212.8 ± 60.3 mL; P = 0.70). Furthermore, they did not find the difference in terms of major adverse coronary events (5.4% vs. 2.6%; P = 0.25). It was suggested that PCI of the CTO in LAD artery could be related to improved LVEF (47.2% ± 12.3% vs. 40.4% ± 11.9%; P = 0.02), but this finding remained hypothesis-generating. Even during prolonged follow-up (median of 3.9 years) of this trial, MACE did not differ between arms (13.5% vs. 12.3%, HR 1.03, 95%CI: 0.54-1.98; P = 0.93). Interestingly, reported cardiac mortality was higher in the CTO-PCI arm (6.0% vs. 1.0%, P = 0.02), while there was no difference in all-cause mortality (12.9% vs. 6.2%, HR 2.07, 95%CI: 0.84-5.14; P = 0.11)[23].
Another randomized trial (the REVASC trial) assessed the effect of CTO recanalization on segmental wall thickening (SWT) (the primary endpoint) and improvement of regional wall motion and changes in left ventricular volumes and ejection fraction (secondary endpoint) in the CTO territory[24]. The change in SWT did not differ between the CTO PCI [4.1 (-14.6 to 19.3)] and non CTO PCI [6.0 (-8.6 to 6.0)] groups (P = 0.57). Similar findings were described for secondary endpoints[24].
EuroCTO (Randomized Multicentre Trial to Compare Revascularization With Optimal Medical Therapy for the Treatment of CTO) trial was the first randomized clinical trial that demonstrated some measurable clinical benefit of PCI for CTO[25]. This prospective randomized controlled clinical trial enrolled 396 patients to compare PCI of CTO with optimal medical therapy, with a 2:1 randomization ratio. This trial showed that at 12 months, there was a greater improvement of Seattle angina questionnaire subscales with PCI vs. OMT for angina frequency (5.23, 95%CI: 1.75-8.71; P = 0.003), and QOL (6.62, 95%CI: 1.78-11.46; P = 0.007). Physical limitation (P = 0.02) also showed improvement in the PCI group. Complete freedom from angina was encountered more frequently with PCI (71.6%) than with optimal medical therapy (57.8%) (P = 0.008). Nevertheless, this study did not show improvement in hard clinical end point event rates in PCI group (although not statistically significant, number of deaths and myocardial infarctions were numerically higher in PCI group). This led investigators to conclude that PCI for CTO leads to a significant improvement of the “health status” in patients with CTO as compared with optimal medical therapy alone[25].
On the contrary, recently presented DECISION-CTO trial[26] showed no difference between PCI and optimal medical treatment in SAQ subscales. This discrepancy with EuroCTO trial results could be explained by study design: in EuroCTO trial there was no influence of non-CTO lesions on endpoints (these lesions were treated before randomization), while in DECISION-CTO trial non-CTO lesions were treated after randomization, which could potentially have some influence on study endpoints[25].
Overall, the amount of high-quality data from randomized clinical trials on positive effects of CTO recanalization is relatively small. Effects are probably limited to improvement in QOL, while it was not possible to demonstrate positive effects on hard clinical outcomes such as mortality and myocardial infarction. However, in modern era of treatment of coronary artery disease, it is becoming more and more difficult to make further improvements in outcomes in the treatment of coronary artery disease, because contemporary medical treatment and overall treatment strategies have already yielded excellent results. It was not possible to demonstrate the clinical benefit of standard PCI (and revascularization in general) over optimal medical therapy alone, in stable coronary artery disease patients[27,28]. This means that task for proving the clinical benefit of PCI for CTO is even more difficult, having in mind inherent lower procedural success rate, higher rate of complications, and lower amount of viable myocardium in the territory of vessel irrigation which usually have developed collateral circulation.
Clinical indications for PCI for CTO
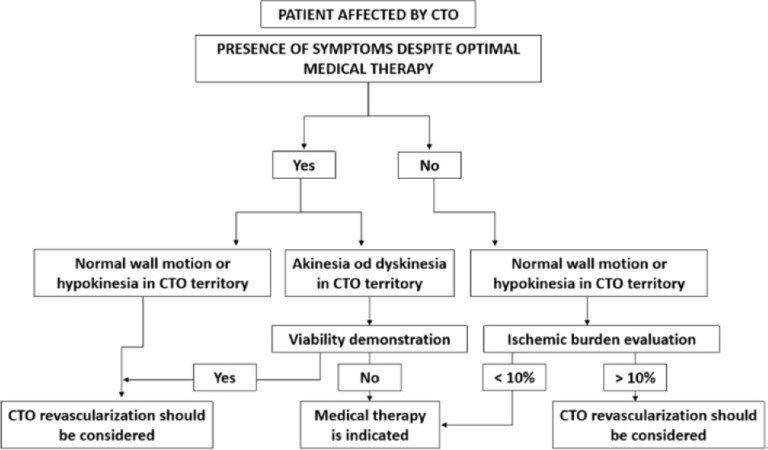
Most important factors that must be taken into consideration before proceeding to CTO-PCI are the presence of symptoms and objective evidence of ischemia, while in cases of left ventricular regional wall motion abnormalities in the CTO territory, objective evidence of viability should be sought. The decision to attempt PCI for CTO should be weighted against the risk of larger amount of administered contrast, longer time of fluoroscopy, and higher rates of MACE compared with PCI for non-CTO lesion[11]. These factors taken together could be shown in the algorithm proposed by the EuroCTO club (Figure 1, modified from[12]). We must emphasize the importance of optimal medical therapy for the control of stable coronary artery disease, which must be the first line of intervention in patients having CTO. In recent 2018 ESC/EACTS Guidelines on myocardial revascularization, it is recommended that percutaneous revascularization of CTOs should be considered in patients with angina that is resistant to medical therapy alone or with a documented large area of ischemia in the territory of CTO (class of recommendation IIa, level of evidence B)[29]. The class of recommendation/level of evidence for PCI of CTO was not changed from the previous version of the Guidelines[30].
Figure 1. Indications of CTO revascularization according to symptoms, ischemia and viability. CTO: chronic total occlusions
The role of SYNTAX score is less suitable for evaluating patients with CTO than for non-CTO patients. CTO lesions are weighted higher (x5) than non-CTO lesions (x2). Therefore, patients with CTOs typically have much higher scores than those with non-CTO lesions for similar disease distribution. Consequently, the high SYNTAX scores strengthen the decision to send CTO patients more often to surgery. Since technical aspects of PCI for CTO have been significantly improved, it might be possible that impact of CTO (vs. non-CTO) lesions for SYNTAX score calculation might be overestimated[31].
Conclusion
Finally, we believe that CTO recanalization performed by experienced operator still has place in interventional practice. The reasonable approach in patient selection would be to take into consideration the following aspects: the burden of symptoms, the extent of ischemia, and the amount of viable myocardium in CTO territory.
Declarations
Authors’ contributionsConception and design of the study, review of the available literature and drafting of the manuscript: Dobric M, Stojkovic S
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2019.
REFERENCES
1. Carlino M, Magri CJ, Uretsky BF, Brilakis ES, Walsh S, et al. Treatment of the chronic total occlusion: a call to action for the interventional community. Catheter Cardiovasc Interv 2015;85:771-8.
2. Sianos G, Werner GS, Galassi AR, Papafaklis MI, Escaned J, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention 2012;8:139-45.
3. Christofferson RD, Lehmann KG, Martin G V, Every N, Caldwell JH, et al. Effect of chronic total coronary occlusion on treatment strategy. Am J Cardiol 2005;95:1088-91.
4. Jeroudi OM, Alomar ME, Michael TT, El Sabbagh A, Patel VG, et al. Prevalence and management of coronary chronic total occlusions in a tertiary Veterans Affairs hospital. Catheter Cardiovasc Interv 2014;84:637-43.
5. Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol 2012;59:991-7.
6. Galassi AR. Retrograde coronary revascularisation in Europe to treat chronic total coronary occlusions. Available from: https://cardiovascularnews.com/retrograde-coronary-revascularisation-in-europe-to-treat-chronic-total-coronary-occlusions/. [Last accessed on 18 Jul 2019].
7. Werner GS, Surber R, Ferrari M, Fritzenwanger M, Figulla HR. The functional reserve of collaterals supplying long-term chronic total coronary occlusions in patients without prior myocardial infarction. Eur Heart J 2006;27:2406-12.
8. Weintraub WS, Garratt KN. Should Chronic Total Occlusion Be Treated With Coronary Artery Bypass Grafting? Circulation 2016;133:1818-25.
9. Galassi AR, Sianos G, Werner GS, Escaned J, Tomasello SD, et al. Retrograde Recanalization of Chronic Total Occlusions in Europe: Procedural, In-Hospital, and Long-Term Outcomes From the Multicenter ERCTO Registry. J Am Coll Cardiol 2015;65:2388-400.
10. Maeremans J, Walsh S, Knaapen P, Spratt JC, Avran A, et al. The Hybrid Algorithm for Treating Chronic Total Occlusions in Europe: The RECHARGE Registry. J Am Coll Cardiol 2016;68:1958-70.
11. Brilakis ES, Banerjee S, Karmpaliotis D, Lombardi WL, Tsai TT, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv 2015;8:245-53.
12. Galassi AR, Brilakis ES, Boukhris M, Tomasello SD, Sianos G, et al. Appropriateness of percutaneous revascularization of coronary chronic total occlusions: an overview. Eur Heart J 2016;37:2692-700.
13. Brilakis ES, Grantham JA, Rinfret S, Wyman RM, Burke MN, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv 2012;5:367-79.
14. Sapontis J, Salisbury AC, Yeh RW, Cohen DJ, Hirai T, et al. Early Procedural and Health Status Outcomes After Chronic Total Occlusion Angioplasty: A Report From the OPEN-CTO Registry (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures). JACC Cardiovasc Interv 2017;10:1523-34.
15. George S, Cockburn J, Clayton TC, Ludman P, Cotton J, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol 2014;64:235-43.
16. Galassi AR, Tomasello SD, Costanzo L, Campisano MB, Barrano G, et al. Long-term clinical and angiographic results of Sirolimus-Eluting Stent in Complex Coronary Chronic Total Occlusion Revascularization: the SECTOR registry. J Interv Cardiol 2011;24:426-36.
17. Stojkovic S, Juricic S, Dobric M, Nedeljkovic MA, Vukcevic V, et al. Improved Propensity-Score Matched Long-Term Clinical Outcomes in Patients with Successful Percutaneous Coronary Interventions of Coronary Chronic Total Occlusion. Int Heart J 2018;59:719-26.
18. Wijeysundera HC, Norris C, Fefer P, Galbraith PD, Knudtson ML, et al. Relationship between initial treatment strategy and quality of life in patients with coronary chronic total occlusions. EuroIntervention 2014;9:1165-72.
19. Safley DM, Grantham JA, Hatch J, Jones PG, Spertus JA. Quality of life benefits of percutaneous coronary intervention for chronic occlusions. Catheter Cardiovasc Interv 2014;84:629-34.
20. Stojkovic S, Juricic S, Dobric M, Nedeljkovic MA, Vukcevic V, et al. Improved Propensity-Score Matched Long-Term Clinical Outcomes in Patients with Successful Percutaneous Coronary Interventions of Coronary Chronic Total Occlusion. Int Heart J 2018;59:719-26.
21. Christakopoulos GE, Christopoulos G, Carlino M, Jeroudi OM, Roesle M, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol 2015;115:1367-75.
22. Henriques JPS, Hoebers LP, Råmunddal T, Laanmets P, Eriksen E, et al. Percutaneous Intervention for Concurrent Chronic Total Occlusions in Patients With STEMI: The EXPLORE Trial. J Am Coll Cardiol 2016;68:1622-32.
23. Elias J, van Dongen IM, Råmunddal T, Laanmets P, Eriksen E, et al. Long-term impact of chronic total occlusion recanalisation in patients with ST-elevation myocardial infarction. Heart 2018;104:1432-38.
24. Mashayekhi K, Nührenberg TG, Toma A, Gick M, Ferenc M, et al. A Randomized Trial to Assess Regional Left Ventricular Function After Stent Implantation in Chronic Total Occlusion: The REVASC Trial. JACC Cardiovasc Interv 2018;11:1982-91.
25. Werner GS, Martin-Yuste V, Hildick-Smith D, Boudou N, Sianos G, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J 2018;39:2484-93.
26. Lee SW, Lee PH, Ahn JM, Park DW, Yun SC, et al. Randomized Trial Evaluating Percutaneous Coronary Intervention for the Treatment of Chronic Total Occlusion. Circulation 2019;139:1674-83.
27. Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16.
28. Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, et al. Percutaneous coronary intervention in stable angina (ORBITA): A double-blind, randomised controlled trial. Lancet 2017;6736:1-11.
29. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2018:1-96.
30. Windecker S, Kolh P, Alfonso F, Collet J-P, Cremer J, et al; Authors/Task Force members. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541-619.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Dobric M, Stojkovic S. Contemporary indications for percutaneous revascularization of coronary chronic total occlusions. Vessel Plus 2019;3:26. http://dx.doi.org/10.20517/2574-1209.2018.77
AMA Style
Dobric M, Stojkovic S. Contemporary indications for percutaneous revascularization of coronary chronic total occlusions. Vessel Plus. 2019; 3: 26. http://dx.doi.org/10.20517/2574-1209.2018.77
Chicago/Turabian Style
Dobric, Milan, Sinisa Stojkovic. 2019. "Contemporary indications for percutaneous revascularization of coronary chronic total occlusions" Vessel Plus. 3: 26. http://dx.doi.org/10.20517/2574-1209.2018.77
ACS Style
Dobric, M.; Stojkovic S. Contemporary indications for percutaneous revascularization of coronary chronic total occlusions. Vessel Plus. 2019, 3, 26. http://dx.doi.org/10.20517/2574-1209.2018.77
About This Article
Copyright
Data & Comments
Data

 Cite This Article 0 clicks
Cite This Article 0 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.